Editor's note: Originally February 6, 2017. Formatting updated February 2024.
Because dental implant componentry is composed of machined parts, implant abutments and fixtures are designed to be mated with minimal vertical misfit between abutment and platform. Brånemark’s original publications1 considered a misfit of 10 microns or less to be acceptable, while some authors have suggested that misfits of 100–150 microns are clinically acceptable.2 This “microgap” needs to be evaluated, however, as literature has suggested that peri-implant bacteria can colonize a gap as small as 1 micron.3
But the threshold used to determine acceptable misfit becomes semantics when a microgap becomes a “macrogap” due to unforeseen factors. When bacteria are able to colonize a macrogap, implant failure can result due to biologic failure such as peri-implantitis.4 In addition, misfit can lead to mechanical failure of the implant system because of factors such as screw fracture and/or implant fracture.5
Recognizing the leading causes of implant abutment misfit can prevent these failures from occurring:
1. The number one reason for prosthetic misfit is usually due to the clinician taking inaccurate impressions that can lead to model distortion. This can also result in the abutment being fully seated on the model, but not in the mouth.
2. Tight contacts from the adjacent dentition can keep the implant abutment from fully seating. This can be a major factor if the time from impression to insertion is long. Teeth are not static and move; thus, the longer the lapse in insertion time, the more likely a shift can occur (figure 1).
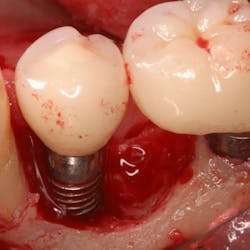
3. Tissue interferences, such as gingiva and/or bone between the abutment and fixture platform, should always be considered (especially in the posterior mandible) when misfit occurs. In addition, calculus, cement, and grafting material can also be lodge between mating surfaces of the abutment and fixture, and prevent seating (figure 2).
4. Mixing parts from different companies can cause component misfit. Third-party parts from “cheaper” implant companies may be used to lower cost, but they don’t always result in complete fit. In fact, implant companies that warranty their parts for replacement often void this warranty if those parts are used in combination with parts from another company (figure 3).
5. The use of engaging abutment in a multiple implant-supported prosthesis can prevent complete seating. (6) According to Chris Salierno, DDS, chief editor of Dental Economics, “If it’s a multiunit case and (for some reason) engaging abutments are used, then it can cause the restoration not to seat. Only nonengaging components should be used for multiunit cases, as they are more forgiving of the slight imperfections inherent with these situations.”
6. Lastly, trying to reinsert an abutment that had been previously misfit onto an implant fixture can cause a macrogap. Implant components can become warped and fatigued, especially if a previous misfit has occurred. When removing large structures, such as hybrids and large-span implant-supported bridges (for purposes of cleaning), one must let the patient know that a misfit could occur when attempting reinsertion.
Many other factors may be responsible for prosthetic-fixture vertical misfit; however, the above-mentioned reasons are the usual culprits. Because vertical misfit can have serious repercussions on the life span of the implant complex, careful attention must be paid to details at the time of insertion. Radiographic confirmation of abutment seating must be performed at the time of insertion as well as throughout the life of the implant.
References
- Brånemark P-I, Zarb GA, Albrektsson T. Tissue-integrated prostheses: Osseointegration in clinical dentistry. Chicago, IL: Quintessence Publishing Company, Inc.; 1985.
- King GN, Hermann JS, Schoolfield JD, Buser D, Cochran DL. Influence of the size of the microgap on crestal bone levels in non-submerged dental implants: a radiographic study in the canine mandible. J Periodontol. 2002;73(10):1111-1117.
- Hermann JS, Schoolfield JD, Schenk RK, Buser D, Cochran DL. Influence of the size of the microgap on crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged implants in the canine mandible. J Periodontol. 2001;72(10):1372-1383.
- O’Mahony, MacNeill SR, Cobb CM. Design features that may influence bacterial plaque retention: a retrospective analysis of failed implants. Quintessence Int. 2000;31(4):249-256.
- Steinebrunner L, Wolfart S, Ludwig K, Kern M. Implant-abutment interface design affects fatigue and fracture strength of implants. Clin Oral Implants Res. 2008;19(12):1276-1284. doi: 10.1111/j.1600-0501.2008.01581.x.
- Oyagüe RC, Turrión AS, Toledano M, Monticelli F, Osorio R. In vitro vertical misfit evaluation of cast frameworks for cement-retained implant-supported partial prostheses. J Dent. 2009;37(1):52-58. doi: 10.1016/j.jdent.2008.09.007.
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a PhD candidate in the field of functional and integrative nutrition. Contact him through his website at drscottfroum.com or (212) 751-8530.