Implant-induced decay or just poor oral hygiene?
When discussing pros and cons of dental implants, many dentists claim that implants are impervious to tooth decay as a treatment benefit. But they often don't discuss the possibility of adjacent teeth getting decay from poor oral hygiene. Dr. Jonathan Ford stresses that each case has different contributing factors and thus warrants different treatment options.
When discussing the pros and cons of having dental implants, many dentists will claim that implants are impervious to tooth decay as a benefit of dental treatment. However, what dentists often don't discuss is the possibility of adjacent teeth getting decay from poor oral hygiene.
In the past few months, more and more cases have presented to my office with decay on teeth adjacent to dental implants. What could be the cause of this?
First, let’s blame the patient. Is his or her oral hygiene sufficient? Is the patient flossing in the area? Is the patient using a crisscross method? Is the patient using any interproximal aids?
Second, have we, as dentists and dental hygienists, talked to our patients about the different methods of proper implant maintenance? Have we mentioned that, due to the emergence profiles of dental implant crowns, there is more surface area to be cleaned and an increased risk for food traps to form? Patients often think implants need less work than their natural teeth, when in fact, implant home care requires more work. Patients can’t just treat implants like they treat their regular teeth. One local periodontist to whom I refer patients states that “implants are not a substitute for teeth; they are a substitute for no teeth.” Think about that distinction for a second. We need to make our patients more aware of that. Is it time we clinicians look in the mirror and see if we are contributing to the problem?
Do the implants have the proper emergence profile? Was the implant placed in an ideal location? A new trend that is emerging is not only to create temporaries or custom healing abutments on anterior teeth for proper emergence profile, but also to create custom healing abutments on posterior implants at the time of placement or uncovering. This allows the tissue to heal in its most ideal fashion. Are posterior teeth round in shape when they emerge from the gingiva? Then why are we using round healing caps? With the help of a custom healing cap, the tissue can contour in a more rectangular fashion when working in the posterior, which gives the dentist more control of emergence profiles and helps to eliminate undercuts and food traps.
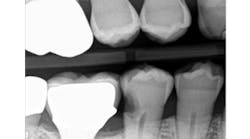
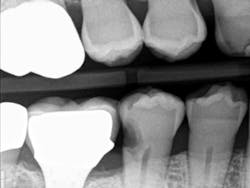
When decay arises on adjacent teeth, dentists must evaluate their treatment options. I have found there is a high degree of difficulty restoring large Class II or interproximal lesions with direct composites, especially when the decay is on premolars. It is much more predictable to restore Class IIs on molars with tight contacts, but it can still be difficult. I have tried full matrix bands and multiple sectional matrix bands, but I can’t create a nice contour with a tight contact. I have even tried traditional composites and bulk fill without great success. See Figures 1 and 2 showing my open contacts with direct composite.
Recently, I changed my protocol for doing Class II dental restorations. I have started using indirect restorations more often. Depending on the size of the restoration, I now use indirect composites, inlays, onlays, and occasionally full-coverage crowns. Using indirect restorations allows one to control the emergence profile of the restoration and also ensures tight proximal and broad interproximal contacts. See Figures 3 through 6.
present at DL line angle not seen on radiograph.
food debris in the contact area.
embrasure space. Distal of No. 28 was restored as well;
not seen in this radiograph.
Every dentist has seen poor dental implant placement and poorly designed implant restorations contribute to adjacent tooth decay. There are also cases of perfectly designed implant restorations that still lead to decay. Each case has a different contributing factor and, therefore, different treatment alternatives to get the job done.