To begin with, there was, without argument, adequate space present for traditional, wider-based platform implants in these sites. So why were mini implants used? As it was understood by the parents, it was the newest technology and standard of care. Their concerns of function, tooth replacement, esthetics, and financial burden were addressed (it was done on trade). This conveys an important point — patients have relatively simple expectations, and when met, they are happy.
ALSO BY DR. STACEY SIMMONS |Managing dental trauma
I felt an obligation to express my concerns to the parents about potential long-term complications.
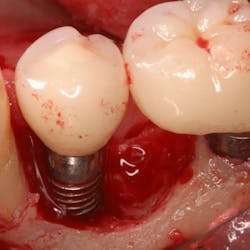
Hygiene. It can be agreed upon that if an implant can’t be kept clean, then the potential for failure and difficulties rise exponentially. A 90-degree angle between the implant and crown is virtually impossible to keep clean and maintain. As amazing as some hygienists are, it is impractical to expect that a curette can get into that space to clean it without making hamburger of the tissue. The implants were cemented on, so they are not easily retrievable. The emergence profile is nonexistent. Do natural teeth look like this? I would submit that when restoring implants, it is our job to mimic the shape and emergence profile of natural teeth as closely as possible. When we don’t, then we lose the inherent cooperation and benefits that the tissue can provide. To help the parents understand this concern, I showed them an example of a traditional implant vs. the “pumpkin on a toothpick” implant. The side-by-side comparison spoke for itself.
vs.
Longevity and function. Premolars don’t get the brunt of mastication forces, but they definitely get their fair share. If the occlusal forces are not centered over the implant just right, then we observe a first-class type of lever that can cause long-term stability issues. It could be argued by some that the 20 mm implant length could render a certain amount of support, but again, the aforementioned point must be referenced — there is/was adequate space for wider based platform implants to be placed.
Esthetics and lack of pain/discomfort. The implants indeed looked like premolars. Making something look good in dentistry is easy. But this is where we have to be careful. Patients don’t know if a crown margin is closed or if a resin is leaking; it is, therefore, up to the provider to maintain a standard of care, own the work, and be behind it 100%. Unless something hurts (and lack of pain does not always mean there isn’t anything wrong), this patient will be happy with the status quo until challenged. That brings me to my last point — financial burden.
In the event that there is failure due to hygiene difficulties, function issues, etc., there will be a time and financial investment for this patient to revisit surgery and restore these teeth, again. Will this patient be pleased? Probably not. Although the work was done on trade, the patient will be getting the short end of the stick, and that does not sit well with me.
With all this being said, there is recognition for the use and application of mini implants in dentistry and my argument is not to undermine the relevance of that use (i.e., mini implant-supported dentures). We must meet the patient’s needs, but just as important, we must set and maintain a standard of care that justifies and supports our decisions should they ever be challenged.
ALSO BY DR. STACEY SIMMONS |All-On-4 treatment option: a case report