The Academy of Osseointegration’s (AO) latest installment of the #AskAO webinar series presented a case for low-insertion torque to yield better clinical results. In the webinar, “Is Tight Right?” Dr. Michael R. Norton, BDS, FDS, RCS (ED), explained the advantages of using an insertion torque of 25 Ncm to facilitate faster osseointegration with immediate placement protocols.
“The industry is driving the direction as far as primary stability and immediate loading. Right now it’s the tighter, the better. We are looking at whether that is the best approach,” explained Dr. Norton.
ADDITIONAL READING | Perio-Implant Advisory 'JOMI Clinical Pearls': Analyzing techniques for maxillary implant placement success
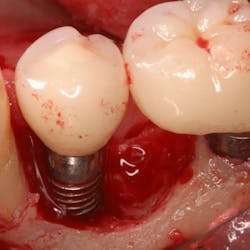
The most common cause for implant failure is excessive micromovement, which is detrimental to osseointegration. The current consensus is implants placed with higher torque (as high as 75 Ncm) yield higher primary stability than those placed with lower torque. Clinicians hit the single target value of insertiontorque for the implant system and test the Peak Insertion Torque (PIT) as a measure of rotational stability.
Dr. Norton, however, does not agree with the principle of the method.
“There isn’t an actual statement that can be made that PIT is a predictor of success,” he said.
Rather, Dr. Norton believes clinicians should use a Resonance Frequency Analysis (RFA) and Implant Stability Quotient (ISQ) as a more accurate measurement of primary stability. RFA measures the axial stiffness between the implant and the bone. Dr. Norton referred to the Al-Nawal et al. (IJOMI. 2006;21:726-732) study that showed, “by contrast the sensitivity of ISQ was such that it could be predictive for failure as this measures axial rather than rotational stability.
ADDITIONAL READING | Ask AO: How do I create a team approach for best implant esthetics?
The current data shows that at three weeks, secondary stability, or biological stability, begins to form. However, Dr. Norton posits that by ratcheting up the primary stability with insertion torques of 75 Ncm or more, clinicians delay biological stability.
Histological studies support his claim suggesting that higher torque at placement contributes to reduced bone-to-implant contact. According to Cha JY et al. (“Multiscale analyses of the bone-implant interface. JDetn Res. 2015;94: 483-490.), “data presented demonstrates that high-insertion torque generates strain in the peri-implant bone that is detrimental to osteocyte survival. High strains constrict blood flow and cause micro-damage to the peri-implant bone, both of which contribute to osteocyte necrosis, extensive bone remodeling, and minimal new bone formation.”
“The truth of the matter is when one is doing immediate loading or immediate temporization, you want that implant to obtain biological stability at the earliest opportunity. You don’t want to delay the healing, and you don’t want to reduce the bone to implant contact. So whilst it may be counterintuitive, it is my belief, and the belief of others who have published on this topic, that a lower insertion torque is actually a better option.”
Often misquoted on this point, Dr. Norton emphasized that he is not saying that high-insertion torque will necessarily prevent osseointegration, but if the osseo-compression creates unfavorable critical pressure in the wrong zone; i.e., crestally, it will result in marginal bone loss over the long term.
He asserted that primary stability should be defined by whatever it takes to allow for successful but rapid osseointegration between implant and bone. He describes this concept as Viable Constraint (vC), or the ability to achieve the combination of rotational stability, while allowing for axial stiffness in the cortical and apical zones, but without compromising bone viability.
Dr. Norton argued that as a profession, clinicians should challenge accepted norms, trust their experience, and look at the evidence. Clinicians should tell the industry what is needed for primary stability, not the other way round.
“Primary stability is NOT insertion torque. We are not carpenters,” he said, “It’s time to think like a clinician. Think viable constraint (vC) and protect the crestal bone.”Register now for the November AO webinar titled "New Perspectives on Vertical Augmentation" with István Urbán, DMD.
The 31st Annual Meeting is set for February 17 to 20, 2016, in San Diego. You can register to attend at www.osseo.org. Follow AO on Facebook and Twitter using #AO2016 to stay up-to-date.