Full-contour screw-retained restorations, sometimes called “screwmentables,” have become very popular. Whether single unit or full arch, the dental restorations are milled zirconia. The term screwmentable came from the fact that the zirconia restorations must be cemented to the interface in order to achieve a precision-milled titanium interface onto the dental implant, not much different than when a dentist cements a crown onto a custom abutment in the mouth. The difference is that the final crown has an occlusal hole that enables the restoration to be retrievable, like a traditional screw-retained porcelain-fused-to-metal (PFM) crown.
The screwmentable option is not new. It was not unusual for dentists to have a custom abutment and crown made with the access hole on a PFM. They would then cement the crown chairside as if it were a regular cementable crown. Eventually, dentists started to cement outside the mouth to prevent the cement from oozing out under the gum. This would be done after the contacts and occlusion were adjusted.
As zirconia restorations proved to be more esthetic, stronger, and better contoured, the desire for implant restorations grew. The first big advancement was the full-arch zirconia bridge. The original motivation was to eliminate porcelain chipping or acrylic wear and breakage. The full-contour zirconia is a monolithic product that should not chip, break, or wear down like hybrids and PFM bridges. The only issue was how to attach the restoration to the implant.
That’s when titanium bases were introduced. A Ti-base is simply a titanium interface of whichever implant system is used. The Ti-base is flat and engages the implant with a little sleeve that extends out to receive the zirconia overframe and attaches via cement. These 12-unit monolithic bridges, which can be screw-retained similar to any cast bridge, were the cause of much rejoicing in the dental industry. Early on, there were some issues with esthetics, translucency, and technique, of course, but today, the Ti-base is a most viable and predictable option. For a single unit, an engaging Ti-base is required, and a single-unit crown is cemented. For a small bridge, a nonengaging Ti-base is required, and the bridge is cemented.
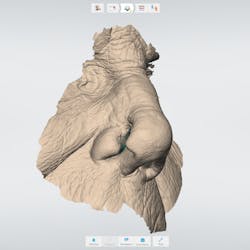
There is one problem that has stirred the dentists’ rumor mill: the debonding of the Ti-base (figure 1). This is an issue that actually does exist. Most of the time, however, debonding is the result of errors by either the lab technician or the dentist.
The fault of the dentist
A single-unit crown should seat easily and be able to be torqued in. The restoration should be checked for proper contacts, occlusion, etc., prior to torquing. Dentists have placed these crowns in the mouth and gone right to torquing them in. What happens is that the contacts may hold the crown in a position that does not allow it to fully seat onto the implant. When the torque driver is used, it pulls the Ti-base down with the screw. It essentially rips the abutment from the crown, breaking the cement bond. When the dentist notices this, he or she will tell the lab that “the crown fell apart in my hand” or claim that it was never cemented at all. The lab will have to recement or, in some instances, make a screw-retained PFM since the dentist no longer has faith in this system.
If the space being filled by the crown is too large, another problem may occur. In this situation, the technician needs to look at the Ti-base. We can see the issue by applying the concept of the crown-to-root ratio to the restoration, a large molar on a regular-diameter implant. The little metal sleeve is not sturdy enough to support the giant crown. In only a few months, the biting force will break the cement, and the crown portion will debond. A better solution is to make a custom abutment that fills up more space and has more surface area to cement to—basically, a full custom abutment that would have a crown cemented onto it by the doctor. This way, when the crown is cemented at the lab, it has extra support and surface area for the cement.
For a full arch, two steps are vital to complete any bridge. The first is a milled prototype that is tried in and verified by the patient and the doctor. The second is a verification jig. This is definitely not a new technique; it was a standard practice for the early Brånemark hybrid frames, for example. If the model is not accurate, the frame will not fit. By verifying the model with the jig and correcting the model, if necessary, we can guarantee a perfect fit. Unfortunately, shortcuts are sometimes taken, such as not using the jig correctly or forgoing the jig altogether. It is imperative to have a passive fit with the jig. If the fit is off, the final bridge will not seat. If the material used to make the jig is soft enough to bend, the rigid bridge will not fit. In these cases, when a bridge is inserted and torqued into the mouth, just like the single tooth with the contacts, a Ti-base is ripped out of the frame. Months later, the doctor will see that a Ti-base is not connected when the bridge is removed. Chances are it was torqued out at insertion, and the bridge has been partially resting on it the whole time.
The fault of the lab
Cement is an obvious culprit in this system. These crowns are mostly zirconia to titanium. Sometimes the crown may be e.max or PFM, and the base may be cobalt chrome. Regardless, the correct cement is a requirement. The crowns are being cemented in the lab. Cementation of restorations is usually done by the dentist. A lab technician may not be aware of proper methodology and material for this purpose. If Ti-bases are not staying bonded, it’s a good idea for the lab to seek out a good account and take a lesson on cementing. It is also very important to make sure that the right cement is used for the purpose at hand. The manufacturer of the zirconia will have recommended cements and materials. They also offer education.
It is mandatory that x-rays be taken at the impression of the implant and again at insertion. The impression coping must be properly seated, as well as the final crown. This can be easily verified on the x-ray. The interface of the Ti-base to the implant should be precise, as should the interface of the crown onto the Ti-base. If they are up at insertion but not in the hand prior to the insertion, then something happened.
A lot of talk has been going on about debonding, and it’s largely exaggerated. Most Ti-base restorations are in the mouth and secure. Simple human error is the main culprit when a problem does occur—not the material.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and dental hygienists for issues relating to periodontal and implant medicine. Exclusive content from an academic perspective centers on complex care, solving clinical complications from a team-based approach through interdisciplinary management.
Steven Pigliacelli, MDT, CDT, is the owner and vice president of Marotta Dental Studio, and has more than 30 years’ experience as a dental implant specialist. He is a faculty instructor in postgraduate prosthodontics at New York University, College of Dentistry, in the department of prosthodontics. He is the founder and past president of the Association of Innovative Dentistry, manages Marotta Dental Studio, and is the technical liaison between the dentist and the laboratory. He also directs the lab’s GPR and Prosthetic Resident Rotation. Contact him at marottadental.com or (866) 627-6882.