Although sinus lifting has been shown to be very predictable with success rates greater than 90%, patients can be somewhat reluctant to accept this procedure due to expense and time. Newer technology, such as growth factors, and noninvasive techniques, such as internal osteotome sinus lifts and/or simultaneous implant placement, have decreased wait time and increased case acceptance. In this article, I will present two cases using newer technologies and noninvasive techniques.
Additional reading …
How to increase safety and reduce complications during sinus lift
Is it time to retire the free gingival graft procedure in light of new alternative tissue grafting materials?
Case 1: Osteotome sinus lift with simultaneous implant placement
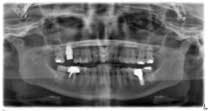
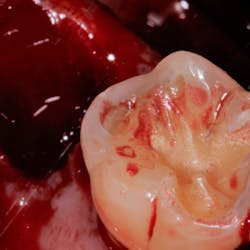
A 53-year-old female with a medical history of hypothyroidism, seasonal allergies, and asthma taking Synthroid and Singula presented to my office with pain in No. 3, failed root canal therapy, and a fracture. The tooth was deemed hopeless and extraction and implant placement was treatment planned. Under local anesthesia, tooth No. 3 was sectioned into three pieces and extracted. The sockets were debrided, filled with gel foam, and closed with chromic gut sutures. Healing was uneventful. The patient did not return for two years for follow-up. A CT scan was taken, which confirmed that approximately5 mm of bone remained below the floor of the sinus. After reviewing the options with the patient, a treatment plan of an internal sinus lift (osteotome), bone graft, platelet-rich fibrin (PRF) and simultaneous implant placement was agreed upon. Under local anesthesia, a full thickness flap with two vertical releasing incisions was performed at tooth No. 3 site. A trephine bur was used to a depth of 4 mm. An osteotome was then employed to infracture the bone core, which remained attached to the Schneiderman membrane. A bone graft consisting of DFDBA, anorganic bovine bone, and PRF was used in the osteotomy to increase the vertical bone height using sequential osteotomes. After sufficient elevation, a 7x9 tapered implant was placed on low speed to 50% of the implant depth. The remaining placement of implant was done with a hand torque on 50 ncm to allow for further expansion of the alveolar housing. A healing abutment was placed using the principles of platform switching. Healing was uneventful, and integration was successful.
Case 1: Implant and osteotome bone graft through the socket with Southern Implant
Case 2: Lateral wall sinus osteotomy with block grafting and platelet-rich fibrin (PRF)
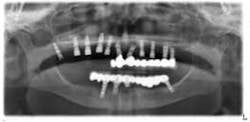
An 81-year-old female with stent placement 10 years ago taking no medications presented with a chief complaint that her old prosthesis broke, and she cannot chew and function. She had a previous bridge consisting of an implant in the No. 1 site combined with the natural teeth and implants in the 8, 9, 14, 15. No. 8, 9 implants were malpositioned with a 35-degree angle and significant mucogingival defects.
Various treatment options were explained to the patient, and a treatment plan consisting of Coldwell-Luc external sinus lift with bilateral block placement in area 5 to 7 and 10 to 12 was agreed upon.
Under local anesthesia, a full thickness flap was elevated from the upper right to upper left posterior segments. Using a piezoelectric handpiece, a buccal window hinge osteotomy was elevated in the maxillary right posterior region. A mixture of DFDBA, anorganic bovine bone, and PRF was placed. A collagen membrane was used to cover the buccal window. Simultaneously, two puros J-block allografts were secured in the 5 to 7 and 10 to 12 region with stainless steel screws (1.6 x 8 mm screws). A mixture of DFDBA, anorganic bovine bone and PRF was placed over each area and covered with PRF sheet and a collagen membrane. Primary closure was obtained with CV-5 Goretex sutures. Healing was uneventful. After six months of healing, six straight implants were placed in sites 3, 4, 5, 6, 11, and 12. Healing abutments were placed at stage I. Healing was uneventful. After four months of healing, six custom abutments were fabricated by his dentist and cover screws were placed on implants 8 and 9 and converted into pontics.
Removing the implants would have created a large buccal defect, which would have created elongated pontics in the maxillary anterior region. The prosthesis was completed, and the patient is stable and highly appreciative of her ability to smile and chew.
Case 2: Sinus lift, bone graft, PRP, and after healing implant placement