By Mark Schlesinger, DDSDespite a plethora of educational resources at our disposal, laser dentistry continues to be largely misunderstood by the dental profession. Unreasonable claims by dental laser manufacturers often fuel speculation and confusion. This article will give a brief overview of some of the benefits of using an Erbium all-tissue laser for surgical therapy and demonstrate realistic clinical benefits of laser treatment. We have various laser wavelengths at our disposal: Diode, Nd:YAG, CO2, and Erbium are the most prominent. Each wavelength has different physical properties that will determine tissue response in reaction to the laser energy. Diode, Nd:YAG, and CO2 are soft-tissue lasers only, while the Erbium family of lasers are soft- and hard-tissue lasers.There are two types of Erbium laser: Er:YAG and Er, Cr:YSGG (Waterlase). Both share a very similar physical profile and, for the sake of simplicity, can be viewed as being interchangeable for periodontal therapy.Top eight surgical benefits of Erbium laser therapy:1. Incision — Larger than a scalpel incision but does not incite nearly the same inflammatory response as it cauterizes small blood vessels. It is also easier to maneuver through interproximal areas, thereby allowing for greater precision with a laser.
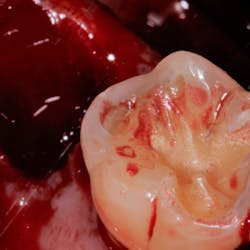
Shows epithelium right after it has been wounded by the laser.
Shows a midcrestal laser incision, no bleeding.2. Flap contraction — Reduced since the need for large flaps is reduced and collagen formation is delayed.
Patient with severe bone loss.
Minimal shrinkage of tissue after surgery.3. Flap reflection — Improved visibility because of coagulative abilities and enhanced access to bony defects.4. Debridement of diseased soft tissue — Although a curette should still be used for gross debridement, a laser is helpful in navigating deep, narrow defects and furcations, because flexible fiber-optic tips allow access to otherwise difficult-to-reach areas. At the proper power settings, this can be done safely without any harm to healthy cementum and bone.
Shows how a furcation can be cleaned out with good access.5. Calculus removal — A laser should be used adjunctively with an ultrasonic or piezo instrument. At a low energy setting, the laser can be used to “paint” over the diseased root surface to help further sterilize it, and to assist in additional removal of invisible adherent toxins.6. Preparation of the root surface — Studies show that a root surface treated with the appropriate laser energy can have greater recruitment of fibroblasts, thereby enhancing regeneration and healing. The exact mechanism is unknown, but may be related to exposing collagen fibrils for cellular signaling.7. Biostimulation — A controversial and exciting issue in the world of medical and dental lasers. Studies show that residual low-level laser energy has the ability to alter cellular metabolic pathways, increasing mitochondrial activity and improving angiogenesis. Researchers are trying to improve regeneration and implant osseointegration using these principles.8. Possibly can act as a membrane barrier — The laser has the ability to wound both the inner and outer epithelium in the periodontal flap, which serves to further enhance regenerative results by excluding epithelial downgrowth into the defect, allowing for new bone and ligament formation to occur.
X-ray before.
X-ray six months after postop. Regeneration using laser, Emdogain, and DFDBA (Demineralized Freeze-Dried Bone Allograft).Erbium lasers are powerful tools that give the clinician the ability to achieve predictable periodontal regeneration, enhance the surgical experience for the clinician, and create a more pleasant healing experience for the patient.It is important to understand that a laser does not replace sound biology, science, and diagnostics. Lasers are not magical. It is foolish to think that you can take a laser light, direct it into a patient’s periodontal pocket, and expect a supernatural result. As with anything else, one must attain extensive training in the use of lasers, and use sound clinical judgment prior to applying laser technology into patient care. Author bioMark Schlesinger, DDS, is a diplomate of the American Board of Periodontology and a clinical assistant professor in the Department of Periodontics and Implant Dentistry at the New York University College of Dentistry. You may contact him at The Diamond Schlesinger Group, nyimplantdentistry.com or nylaserinstitute.com.