I’ve had the pleasure of talking with dentists all over the world. In my lectures I often ask, In dental school, what were you taught causes bruxism? I will almost always have one or two dentists say something to the effect of “occlusal interferences,” but the vast majority of the dentists in the room will shout out, “STRESS!”
They, of course, are referring to emotional stress, and, indeed, there is evidence that some people will grind and clench their teeth episodically due to stressful life events.
However, this “stress theory” was never very satisfying for me. Directly out of dental school, I entered a practice limited to the treatment of temporomandibular disorders and craniofacial pain. As you might imagine, I have seen lotsof patients over the years who suffer from bruxism. With some of them, it was quite clear that emotional stress played a significant role in their pain, dysfunction, and parafunction. But for most of my patients, emotional stress didn’t seem to be the key. I even had (and still have) my patients fill out psychological screening tests to help me isolate those with issues that they weren’t necessarily going to share with me in their medical history. The majority of my patients didn’t show excessive stress levels on these objective questionnaires.
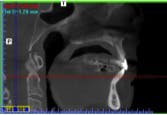
Then I started treating patients with obstructive sleep apnea. I started making connections. I started looking more closely at the bruxism-related literature. Then I bought a cone beam CT and was able to visualize the airway. I started making more connections. I started looking at more literature and testing my theory that nocturnal bruxism (including clenching and grinding) was related to an attempt by the patient’s subconscious to protect the airway during sleep.
Think about it. Why do you see so many patients with anterior wear? The next time you see patients with anterior wear, ask them if they snore. Look at their oropharyngeal airway. If you see large tonsils and a long uvula, or you can’t see the back of their throat because their big tongue is in the way, start asking them how they sleep. If they have grooves on their tongue from their tongue trying to escape the confines of their mouth to get out of the airway, think about the possibility of sleep apnea.
Now, you may think that obstructive sleep apnea is more common in overweight, older men ... and you’d be correct. However, when a thin woman, say in her 40s, goes in to the doctor and complains of nonlocalized pain, poor sleep, and fatigue, she walks out the door with a prescription for an antidepressant — not usually a referral for a sleep study. The woman I just described is also the classic “TMJ patient.” She also happens to be the classic “fibromyalgia patient,” “chronic fatigue syndrome patient,” and, of course, “depressed patient.”
Today, when such a patient comes into my office by referral for a “TMJ problem,” I evaluate him or her for a possible sleep disordered breathing problem. I look at the patient’s teeth for wear patterns, and I examine the oropharyngeal airway. When indicated, I refer these patients for a formal evaluation with a sleep doctor. Often, these patients participate in a sleep study, and I find that more than 90% of my referred patients are diagnosed with obstructive sleep apnea. And here’s the kicker — when obstructive sleep apnea is treated (with either CPAP or an oral appliance), the bruxism is reduced or stopped, the patient’s pain lessens, and function returns to normal.
Interesting! So maybe these patients ARE grinding and clenching their teeth due to stress ... the stress of suffocating in their sleep!
And this doesn’t just apply to adults. The literature shows that children who brux and snore are extremely likely to have sleep apnea. Snoring and bruxism in children are also linked to ADHD, enuresis, and poor school performance. When these children have their tonsils and adenoids removed, there tends to be a significant reduction in bruxism and the other sleep apnea-related signs and symptoms.
In adults, use of CPAP for sleep apnea has been shown to reduce bruxism activity, as has the use of mandibular advancement appliances. Basically, if you allow the patient to breathe, the body’s need to protect the airway through posturing the jaw forward (anterior wear), clenching (keeping the jaw from falling backwards), or bruxism in general (activating muscles that help open the airway) is reduced or eliminated.
In my next article, I’ll tell you what to look for when screening your patients for possible sleep apnea-related bruxism. In the meantime, just realize that maybe your patients (and maybe even you) grind their teeth when they sleep due to stress ... the stress of not breathing!
Author bio
Jamison Spencer, DMD, MS, is the director of the Craniofacial Pain Centers of Idaho and Colorado. His practices are limited to helping people with obstructive sleep apnea and TMJ/craniofacial pain disorders. He completed his DMD degree at Southern Illinois University, and an MS degree in craniofacial pain through Tufts University. He is a diplomate of the American Board of Craniofacial Pain and a diplomate of the American Board of Dental Sleep Medicine. Dr. Spencer is adjunct faculty at Tufts University in its Craniofacial Pain Center, and at Boise State University in anatomy. He is currently the immediate past president of the American Academy of Craniofacial Pain. You may contact Dr. Spencer by email at [email protected], or visit his website at www.JamisonSpencer.com to find out where he will be lecturing next.