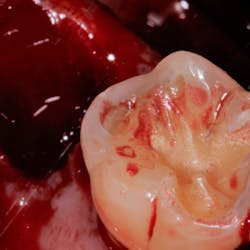
Extravasation of blood during a traumatic event such as dental surgery causes the formation of a fibrin-rich clot. The clot consists of coagulated blood and aggregated platelets within a cross-linked fibrin network. Among the important functions of the clot are its role as a reservoir of growth factors and cytokines that are released by the degranulation of activated platelets. The clot also serves as aprovisional matrix for cell migration. The growth factorsand cytokines present in the fibrin clot provide some of the start signals for wound repair.During the first one to two days there is recruitment of neutrophilsto the wound site, followed by epithelialization,granulation tissue formation, and angiogenesis.The neutrophilscleanse the wound of foreign particles, debris, and bacteria. They remove this matter via the release of destructive enzymes and toxic oxygen products by the oxidative burst phenomenon. Hence, increasing numbers of contaminating bacteria in the wound increase the potential for neutrophil-mediated tissue destruction. Neutrophils also serve as a source of pro-inflammatory cytokines providing signals that activate adjacent fibroblasts and keratinocytes. By day three the neutrophils are phagocytosed either by macrophages or fibroblasts. Peripheral blood monocytes that continue to be recruited into the wound site become macrophages upon activation. Fibrin, along with fibronectin in the clot, acts as a provisional matrix for the influx of monocytes and fibroblasts. Macrophages continue cleansing the wound and releasing cytokines and growth factors. Thus, the wound repair signals initiated by degranulating platelets and neutrophils are maintained by macrophages.
The wound begins re-epithelialization as early as day two when epithelial cells begin to migrate beneath the superficial layer of polymorphonuclear cells (the polyband), which forms beneath the blood clot. Epithelial cells migrate at a rate of 0.5 mm to 1.0 mm per day toward the center of the wound. This process peaks by day seven, forming a new basal lamina and matrix, which is mediated by the mobilization and adhesion of integrins to the provisional matrix and adjacent wound debris by means of migrating keratinocytes. Once re-epithelialization is complete, the components of basal lamina are deposited in a sequential manner starting from the wound margin, and the epithelial cells revert to their normal phenotype. Several growth factors seem to be key players in regulating the proliferation of keratinocytes in healing wounds. Among these factors are epidermal growth factor, transforming growth factor alpha, heparin-binding epidermal growth factor, and keratinocyte growth factor.
The migration of epithelial cells through the clot and provisional matrix requires the formation of a pathway through these obstacles. This necessitates matrix degradation and wound cleansing. The process is mediated by the fibrinolytic enzyme, plasmin. Plasmin is derived from activated plasminogen in the fibrin clot. The importance of plasminogen in wound re-epithelialization is demonstrated by the lack of re-epithelialization of wounds in mice where the plasminogen gene has been knocked out. In addition to plasmin, matrix metalloproteinases cleave and degrade collagens found in the matrix and basal lamina, thus aiding cell migration.
Granulation tissue formation may begin by day four. It consists of new capillaries, fibroblasts, macrophages, and loose connective tissue. It is a reservoir of cytokines and growth factors, as well as signaling molecules, mitogens, and chemotactic factors. The fibroblasts found in the granulation tissue are actively laying down the extracellular matrix. This process has been referred to “fibroplasias.” Studies have shown that when purified growth factors were deposited in granulation tissue, the wounds showed accelerated granulation tissue formation and wound healing (Lynch et al., Sporn et al.). It is also important to note that the activities of certain cell types and the nature of the extracellular matrix environment influence the final phenotype expression by the cells.
As wound healing progresses, the provisional matrix is replaced by a new, collagen-rich matrix synthesized by fibroblasts migrating into the wound. The synthesis of specific extracellular matrix molecules by fibroblasts in the wound is regulated by transforming growth factor-b1 and other factors such as insulin-like growth factor, interleukin 1a and 1b, interleukin-4, and vascular endothelial growth factor. Once the collagen matrix has been laid down, unknown signals down-regulate the process. About seven to 10 days after wounding, some of the fibroblasts in the wound transform into myofibroblasts and express a smooth muscle actin. Such transformation allows these myofibroblasts to generate a strong contractile force that is responsible for wound contraction. In the final stages of fibroplasias, the myofibroblast and fibroplast numbers are decreased by apoptosis. It is interesting to note that wounds in embryos also heal via myofibroblast contraction; however, unlike in adult wounds, they heal without scarring during contraction. This may be explained by the low and transient expression of TGF-β1 in embryos. Shah and colleagues (1992) showed that antibodies can neutralize the effects of TGF-β1 in healing wounds, and thereby reduce scarring.
The term “granulation tissue” in wounds was coined in reference to the red granular appearance of new blood vessels that invade the healing connective tissues. The process of angiogenesis or formation of new blood vessels begins early in wound healing. It is paramount to healing. Various growth factors are key players in this process, including FGF-2, which is synthesized by macrophages and damaged endothelial cells, while VEGF is induced in wound-edge keratinocytes and macrophages. Broadley and colleagues (1989) showed that when FGF-2 is absent, there is a blockage of wound angiogenesis. As in the case of fibroblasts and keratinocytes, the endothelial cells also have to upregulate specific integrins (aVb3) on their surface in order to respond to angiogenic signals. All the signals that induce proliferation, migration, and phenotype expression in endothelial cells have not been completely elucidated. It is clear that angiogenesis is a complex process and relies on the availability of an appropriate matrix in the wound. The process of revascularization and angiogenesis begins three to four days after wounding and proceeds for about 10 to 15 more days. As in the case of fibroblasts, endothelial cells involved with wound angiogenesis also undergo apoptosis during the ultimate maturation of the matrix characterized by regression of capillaries.
Recent discoveries in the area of biologics that have been made in the last two decades can be applied to our understanding wound healing in order to potentiate and enhance the process, particularly for those in whom it is impaired. For example, systemic conditions such as diabetes may be accompanied by reduction in the availability of some of the growth factors; in these cases, supplementing the appropriate growth factor may be beneficial. In addition, modifying collagen metabolism with chemically modified tetracyclines (e.g., CMT-2,6,8), as has been investigated by Golub and colleagues, needs further research before it can recommended for improved wound healing in diabetics. Using products such as enamel matrix derivative for regenerative procedures can also have a supplemental effect by enhancing wound healing following surgery. Evidence suggests that PDL cells exposed to EMD switch their phenotype by increasing expression of growth and differentiation factor related genes, including TGF-β, which is active in key healing events such as extracellular matrix synthesis and fibroblast and macrophage chemotaxis. Products like Gem21s, which is composed of platelet-derived growth factor in a tricalcium phosphate, promote nonspecific mitogenesis and chemotaxis of periodontal ligament fibroblasts. Bone morphogenic proteins (e.g., BMP-2) enhance and promote osseous healing by promoting morphogenesis and angiogenesis. The start and stop signals for the many intricately coordinated events are still not completely understood. A thorough understanding of these signals and their effects on differential gene expression will enable manipulation of wound healing cascade that can lead to the invention of biomimetic technology and regeneration of damaged tissues.
Author bio
Helen Rozenfeld, DDS, is a postgraduate periodontology resident at the SUNY Stony Brook School of Dental Medicine. She received her DDS at SUNY Stony Brook, where she was elected to membership in Omicron Kappa Upsilon, the National Dental Honor Society. She has been the recipient of numerous awards including the American Academy of Periodontology Award, Blasco C. Gomes Periodontology Scholarship, Dr. Richard J. Oringer Periodontology Award, American Association of Oral and Maxillofacial Surgeons Award, and The Charles and Maria Ryan Scholarship for Future Academicians. Dr. Rozenfeld is currently the Stony Brook Student Ambassador for the American Academy of Periodontology Foundation.
References
Aukhil I. Biology of wound healing. Periodontology2000. 2000; 22:44-50.
Broadley KN, Aquino AM, Woodward SC, Buckley-Sturrock A, Sato Y, Rifkin DB, Davidson JM. Monospecific antibodies implicate basic fibroblast growth factor in normal wound repair. Lab Invest. 1989; 61:571–575.
Golub LM, Ramamurthy N, McNamara TF, Gomes B, Wolff M, Casino A, Kapoor A, Zambon J, Ciancio S, Schneir M, Perry H. Tetracyclines inhibit tissue collagenase activity. Journal of Periodontal Research. 1984; 19:651–655.
Howell TW, Fiorellini JP, Paquette DW, Offenbacher S, Giannobile WV, Lynch S. A phase I/II clinical trial to evaluate a combination of recombinant human platelet derived growth factor-BB and recombinant human insulin-like growth factor-I in patients with periodontal disease. J Periodontol. 1997; 68:1186–1193.
Lynch SE, Colvin RB, Antoniades HN. Growth factors in wound healing. Single and synergistic effects on partial thickness porcine skin wounds. J Clin Invest. 1989; 84:640-646.
Martin P. Wound healing- aiming for perfect skin regeneration. Science. 1997; 276:75–81.
Rose LF, Periodontics: Medicine, Surgery, and Implants. Mosby 2004.
Ryan ME, Usman A, Ramamurthy NS, Golub LM, Greenwald RA. Excessive matrix metalloproteinase activity in diabetes: inhibition by Tetracycline analogues with zinc reactivity. Curr Med Chem. 2001; 8:305-316.
Shah M, Foreman DM, Ferguson MWJ. Control of scarring in adult wounds by neutralizing antibodies to transforming growth factor-b. Lancet. 1992; 339:213–214.
Sporn M, Roberts AM. Peptide growth factors and inflammation, tissue repair, and cancer. J Clin Invest. 1986; 78:329–332.
Stahl SS, Froum SJ, Kushner L. Healing responses of human intraosseous lesions following the use of debridement, grafting and citric acid root treatment. II. Clinical and histologic observations: one year postsurgery. J of Periodontol.1983; 54(6):325-338.
Tarnuzzer RW, Schultz GS. Biochemical analysis of acute and chronic wound environments. Wound Repair and Regeneration. 1996; 4:321–325.