Proper embrasure form between teeth and restoration is critical for both proper papilla formation as well as hygiene/cleanability. Embrasure form depends on multiple factors, including tooth position, periodontal status of teeth, tooth contact, and crown morphology. Open embrasures contribute to retention of food debris and may have an adverse effect on the periodontium.
RELATED |Two fundamental etiologies of open embrasures
RELATED |A review of mechanical dental plaque control
Implant replacement for missing teeth is now becoming the standard of care. Successful rehabilitation with dental implants includes stability of bone level, function, esthetics, and overall patient satisfaction. Below is a case review in which we managed to meet all criteria of success except for patient satisfaction; the patient complained that food was getting stuck between her implant and natural crown.
Figs. 1-3: Decayed root No. 19, hopeless prognosis. Treatment plan included single implant fixture with implant-retained PFM.
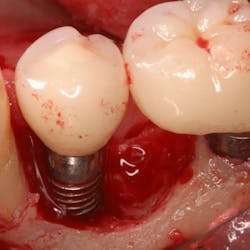
Figs. 4-6: Extraction with immediate implant placement showing buccal/lingual, mesial-distal placement (Fig 4). A 5.2 WP x 10 mm fixture placed to level of buccal crest (Fig 5, 6).
Figs. 7-8: At uncovering, note slight exposure of cover screw with approximately 1 mm keratinized tissue (Fig. 7). A 2 mm collar used as healing abutment. Normal bone remodeling noted and implant appeared well integrated.
Was this patient’s open embrasure form a mistake made by the restorative dentist? A bad tissue model poured by the lab? Upon closer review of the case, it was multifactorial, including surgical error:
1. Inadequate depth of implant placement did not leave the restorative dentist adequate room to develop a proper emergence profile. Should he have tried to close the space, the emergence profile would have become more "flat," making hygiene efforts more difficult.
2. The M-D span for No. 19 is wider than the patient’s natural molars ... for a single implant replacement, the fixture needs to be placed deeper to develop a proper, gradual emergence profile. Two fixtures or a wider platform may have even been considered to close the embrasure space.
3. Slight mesial inclination of tooth No. 18 may also be a factor.
How deep should an implant be placed then? The answer is as deep as necessary, but as shallow as possible. Adequate depth is important for esthetics and development of proper emergence/embrasure forms. But we also want to keep the platform as shallow as possible to allow for cleanability and long-term maintenance. Treatment planning and proper patient education are key (Figs. A-H)!
Patient presents with unrestorable tooth No. 30 (Fig. A). Tooth was extracted and a 5.0 x 10 fixture immediately placed — mesial/distal and buccal/lingual position shown (Fig. B). Implant was placed 1 mm below the buccal crest. A 2 mm healing collar was placed to prevent bone overgrowing the height of the platform (Fig. C & D). Final restoration demonstrates excellent crown contour and embrasure form — there is adequate space for proper maintenance without food entrapment (Fig. E and F). Cement is not an issue as the final restoration is screw retained (Fig. G) with excellent bone levels and proper emergence profile demonstrated by a periapical radiograph (Fig. H).