Accidents happen! It is inevitable that all of us will encounter and treat dental trauma. These situations can be a challenge because these patients are in pain, they are scared, nervous, and they need you — NOW! You as a provider realize the immediate demand of your time, and you are also well aware of your already full schedule and commitments.
ALSO BY DR. STACEY SIMMONS |All-On-4 treatment option: a case report
Improving treatment outcomes in traumatic dental injuries is partially dependent on our ability to assess the situation and render the appropriate care. Although each situation is unique, there are protocols that can be used as a guideline to help us determine the appropriate course of action.
Here are some general recommendations:
• Classify the dental injury — i.e., enamel fracture, crown fracture with or without pulpal involvement, root fracture luxation (concussion, subluxation, lateral, extrusive and intrusive), avulsion, and fracture of the alveolar process.
• Do a thorough assessment that includes history of the injury, TMJ evaluation, radiograph and neurological exam, and occlusal assessment.
• Perform immediate treatment goals: control bleeding and pain, preserve pulp vitality (especially in immature permanent teeth), and preserve PDL cell vitality
• Assess the need for splinting, which is dependent on the nature of the injury (approximations)
a.Root fracture — 3 months
b.Alveolar process fracture — 6-8 weeks
c.Luxation — 2-3 weeks. If alveolar is involved, then 6-8 weeks
d.Avulsion — 2-4 weeks
Definitive treatment protocols depend a great deal on what happens over the course of time once the initial treatment goals are completed. Depending on the nature of the injury and condition of the apex, a follow-up appointment with the patient is mandatory to allow for an assessment to determine whether or not calcium hydroxide therapy should be initiated. Long-term complication considerations include ankylosis, arrested alveolar process growth, and inflammatory root resorption. A frequent recall should be established to assess for these and other possibilities.
ALSO BY DR. STACEY SIMMONS |Are you sure I have a cavity?
Case reports
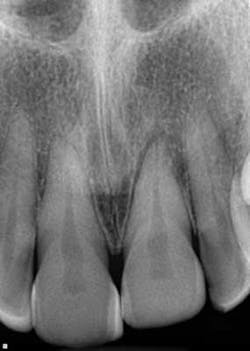
A healthy 7-year-old female presented directly from school with her father stating that she fell off the monkey bars. This was her first visit to the dentist. Initial exam revealed that tooth No. 8 was partially avulsed (Fig. 1) with only a slight attachment to the gingiva. All other teeth appeared clinically normal. Radiograph assessment revealed a large open apex on No. 8. The patient was given a local. The clot was removed and the area irrigated with a saline rinse. Next, the tooth was gently repositioned in the socket with slight compression of facial and lingual alveolar processes. A nonresilient wire splint was placed from NOs. 7 through 9. The patient was given an Rx of antibiotics for potential infection. A one-week assessment revealed a significant decrease of swelling with No. 8 appearing fairly stable. After eight weeks, tooth No. 8 had a slight delay to cold testing with all other teeth testing normal. The splint was removed. It was discussed with the father that the delayed response could be attributed to the healing of pulp or potential pathology. A two-month follow-up was recommended.