Introduction
Vertical dimension of occlusion is used to denote the superior inferior relationship between the maxilla and the mandible when teeth are in maximum intercuspation. When vertical dimension is decreased significantly, either via loss of teeth or parafunction, the result can be a collapsed bite.
RELATED READING |Harmony in prosthodontics
As vertical dimension is lost, the proportions of the face are altered; one’s chin becomes recessed, the lower half of the face may look short, and the angles of the mouth can develop chelitis. Loss of vertical dimension results in facial collapse, wrinkles by the nasolabial fold, and appearance of compressed and thin lips, which makes one appear older.
RELATED READING |All-On-4 treatment option: a case report
Dentures can be fabricated to correct a collapsed bite and increase vertical dimension in patients with missing teeth. Alternatively, vertical dimension can also be increased via an acrylic bite plate and/or fixed prosthodontic work.
Case report
A 60-year-old male patient presents to the dental office with the following chief complaint: “My lower teeth are getting shorter.” Upon visual extraoral examination, the patient had difficulty keeping his lower jaw still at all times; upon sitting still, the patient’s jaw tremors from side to side. It appears as though the patient may have Parkinson’s disease; however, the patient states that his medical conditions only include diabetes and hypertension. He is taking lisinopril to control his blood pressure. He denied tremors or Parkinson’s.
Initial dental examFig. 1: Patient’s panographic radiograph
Fig. 2: Bitewing and periapical radiographs
Patient presents with multiple existing root canals and fixed prosthodontic work.
Fig. 3: Intraoral preoperative photographs
The patient has ground through the porcelain on the lingual surfaces of the crowns on Nos. 6, 7, and 9.
The occlusal surfaces of the posterior teeth and incisal edges of the anterior teeth in the mandibular arch have considerable wear due to the fact that the patient is a bruxer. He is grinding natural tooth structure in the mandible against porcelain in the maxilla. Enamel is softer than porcelain and wears away quicker when the patient functions and grinds his teeth.
Fig. 4: Treatment plan
The pulp in the patient’s teeth had receded considerably and, therefore, endodontic therapy was not necessary prior to preparing his teeth for full-coverage PFM restorations.
Preliminary impressions of the patient’s maxillary and mandibular arch were taken and poured up. A wax-up of the mandibular arch was created, opening the patient’s bite 3 mm. A PVS matrix was then fabricated on top of the wax-up.
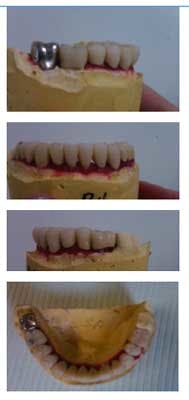
Fig. 5: Intraoral photographs, temporaries
The PVS matrix was then used to build up the occlusal surfaces posterior teeth and incisal edges of anterior teeth in the mandibular arch with composite and open his bite 3 mm. The patient was kept in these temporaries for five months. The patient would return to the office once a month to assess his TMJ and occlusion. Every month, the patient denied TMJ symptoms.
Fig. 6: Teeth prepared for PFMs
After preparing the teeth for full-coverage PFMs, the patient returns to the office to try in the metal copings. Copings fit appropriately and were sent back to the dental laboratory for porcelain bisque bake.
Fig. 8: Bisque bake
Fig. 10: Inserted full-coverage PFMs
Upon completion, a maxillary day and night guard was fabricated for the patient, and he was advised to constantly wear this device.