Microscopes have been used for decades in various medical specialties and have recently been introduced to endodontics (Carr). Benefits of this technology include enhanced visibility and lighting, detection of coronal and radicular cracks and fractures, patient education with pictures displayed on the monitor, location of calcified and additional canals, bypassing ledges, removal of separated instruments, and viewing perforations for repair. One of the main reasons noted for failure of root canal therapy in maxillary molars is failure to locate a second mesiobuccal canal. Weller and Hartwell, in their retrospective clinical study, recorded a second mesiobuccal canal in 39% of their sample of maxillary first molars (Weller). The incidence of a second mesiobuccal canal has been reported to be between 18% and 96.1% with the aid of the dental microscope (Kulild, Buhrley). Other variations include three, four, and five roots and unusual morphology of root canal systems within individual roots, anatomy often undetected without the use of a microscope. The following case highlights unusual anatomy within a maxillary first molar.
ADDITIONAL READING |Periodontal abscess, endodontic abscess, or a combination: How to decipher
Case report 5-canal molar
A 53-year-old female presented for a consult after an evaluation during an emergency visit to her GP, upon which she was referred to City Endodontics for an endodontic consult.
The patient presented with no known drug allergies. She was taking Aleve (naproxen sodium) 220 mg p.o. q8h prn pain. The patient suffered from sciatica (slipped disc which creates pain that radiates along the path of the sciatic nerve, branching from the lower back through the hips and buttocks and down each leg) and experienced bouts of extreme pain in her left leg and lower back when positioned abnormally for long periods of time. She noted that she could not withstand visits longer than one hour and could not recline beyond 145 degrees.
She presented with a history of lingering pain to cold liquids and a spontaneous, throbbing ache. Tooth No. 3 had a large MOD, amalgam restoration placed "several" years ago by a GP from whom she no longer received care. She noted that discomfort began about one month prior to her current visit. The pain had increased, and she rated it a 6 out of 10 on a visual analog pain scale. The extraoral exam was within normal limits, there were no signs of asymmetry, no edema, no erythema, no lymphadenopathy, no clicking, crepitus, or deviation of mandible noted during the TMJ exam. Muscles of mastication were not tender to palpation.
The intraoral exam of the posterior, right maxillary gingiva appeared normal with no associated edema or erythema. Generalized recession was visible 2-3 mm apical to the CEJ. No. 2 showed occlusal amalgam with intact margins, No. 3 MOD amalgam with compromised margins along occlusal cavosurface, and No. 4 DO amalgam presented with open margins with recurrent caries near the distal CEJ region.
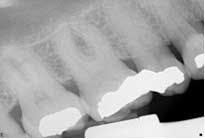
Radiographic interpretation showed the maxillary sinus, which appeared to be superimposed over the apex of teeth Nos. 2 through 4. In the radiograph No. 2 showed a shallow occlusal radiopaque restoration consistent with the appearance of amalgam. The mesial aspect of the tooth was visible with the mesiobuccal root showing. A radiopaque structure appeared to be within the chamber consistent with the appearance of a pulp stone. An apparent widening of the PDL at the apex of the tooth was visible. Tooth No. 3 showed a radiopaque MO restoration within 2 mm of the pulp chamber. The tooth appeared to exhibit three roots with the distal root appearing to be “bulbous” in presentation, and multiple periodontal ligaments were visible and associated with this root. The presentation of multiple periodontal ligaments is an indicator that multiple canals may be present within a root (Beatty). No. 4 showed a DO radiopaque restoration consistent with the appearance of amalgam; the canal space was visible to the junction of the middle/apical third in which it became obscure. The distal root aspect of tooth No. 5 appeared to be partially visible. (Fig. 1)Fig. 1: PA of maxillary posterior
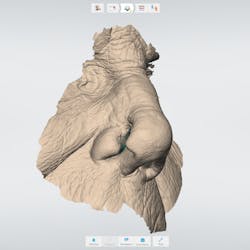
Treatment NSRCT No. 3: 20% topical benzocaine was applied to buccal and lingual injection sites for one minute after being wiped dry with 2x2 gauze. 2x1.8 mL carpules (72mg) 2% lidocaine, 1:100K epinephrine (36 micrograms) buccal (PSA/MSA), and palatal infiltration were administered. Rubber dam isolation was achieved and a bite block positioned to prop the patient’s jaw open. The procedure was performed with the DOM. A bite block was used to help position the patient's jaw in an open position to aid in the initial endodontic access but removed after access was refined. The DOM was positioned at an angle of 60 degrees to facilitate operations while standing over the patient. (Fig. 2) Four canals (MB/MB2, DB, and P) were located with use of anatomical landmarks, DOM, and ultrasonic excavation. Irrigated with 20 mL 6% NaOCl (aids in tissue dissolution, mechanical flushing, lubrication, organic smear layer removal, anti-microbial), 20 ml 17% EDTA (chelating agent, lubricant, removal of inorganic smear layer) RC-Prep (chelating agent, surfactant, lubrication) used with #6-25K-files to resistance. Gates Glidden burs used #2, 3, 4, 1 w/RC Prep. The working length was obtained by close evaluation of preop radiograph and use of an apex locator (RootZX II). The crown down instrumentation (CD) technique was used with Hyflex rotary files (Coltene) and recapitulation was employed throughout the entire procedure. Canals were dried with paper points and Ca(OH)2 (Metapaste) placed within all canals (anti-microbial, tissue dissolution, anti-inflammatory, hygroscopic properties, anti-resorptive and anti-endotoxin agent). Following treatment cotton pellet/Cavit g were placed and postoperative instructions (POI) given verbally and written. The patient was scripted Motrin 600 mg and dispensed 12 tabs, with instructions to take one tab every six hours p.o. for pain (anti-inflammatory, analgesic). The patient was dismissed in stable condition.
Fig. 2: Dental operating microscope (Global)
Rx: Motrin 600 mg, dispense 12 tabs, take one tab every six hours p.o. for pain (anti-inflammatory, analgesic). A postoperative call was placed later that evening and POI reinforced. The patient was noted as being in stable condition.
Second visit The patient returned to City Endodontics for treatment asymptomatic two weeks later. Rubber dam isolation and access were modified with the DOM; exploration of the distal anatomy was revisited. The distal canal was troughed with a fine diamond tip from an ultrasonic machine (Coltene), and a disto-buccal (DB2) canal located with the aid of the NaOCl 6% bubble test and anatomical landmarks. The DB2 canal was cleaned and shaped to length using same technique used for the other canals at the initial visit. The apex locator Root ZX II was used to confirm presence of an additional canal and reconfirm length for other canals. A check film was taken with files in all five canals to verify presence of five separate orifices and apices. A master cone for all five canals with gutta percha fit to working length was exposed. (Fig. 3)Fig. 3: Master cone fit radiograph of tooth No. 3 highlighting five canals
Figs. 4 and 5: Radiographs of tooth No. 3: Five-canal molar with two mesial and two distal canals present
The obturation technique included warm vertical condensation with continuous wave and AH-plus sealer and backfilled all the canals to their respective orifice. Cotton and cavit g temporary restoration were again placed more than 3 mm from the occlusal surface to prevent coronal micro-leakage in the access cavity. The occlusion checked, postoperative instructions were written and verbally given. Two periapical radiographs were exposed to illustrate the unique anatomy. (Figs. 4 and 5)
References
1. Carr GB. Microscopes in endodontics. J Calif Dent Assoc. 1992;20:55-61.
2. Kulild JC, Peters DD. Incidence and configuration of canal systems in the mesiobuccal root of maxillary first and second molars. J Endod. 1990;16:311-317.
3. Buhrley LJ, Barrows MJ, BeGole EA, et al. Effect of magnification on locating the MB2 canal in maxillary molars. J Endod. 2002;28:324-327.
4. Beatty RG. A five-canal maxillary first molar. J Endod. 1984;10:156-157.