The JOMI Spotlight is a regular column in Surgical-Restorative Resource that discusses articles from the Journal of Oral and Maxillofacial Implants (JOMI) — the official journal of the Academy of Osseointegration (AO) — as reviewed by a member of the Academy’s Young Clinicians Committee (YCC). Quintessence Publishing publishes JOMI.
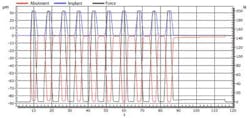
After reviewing the November/December issue, I want to start by revisiting the implant-abutment interface, trying to quantify micromotion for a variety of implant-abutment combinations. The experiment mimicked occlusal loading of the implants while utilizing a new technique that accessed both the implant shoulder and the abutment to determine the displacement between the two. Micromotion can contribute to prosthetic failure, such as screw or abutment loosening (with an occurrence of 12.7% in implant-supported single crowns) and screw fractures. The mean values of micromotion found were highly variable, ranging from 1.52 to 94 um. A significant relationship was found between tightening torque and micromotion. Karl/Taylor et al. tested the Straumann Standard implant tightened at 5, 15, and the recommended 35 Ncm, and found significantly less micromotion at the recommended 35 Ncm. A similar micromotion was found for the Strauman provisional abutment tightened at the recommended 15 Ncm, implying that the optimal tightening torque is abutment/manufacturer-specific. When evaluating high-value implant systems with low-cost clones vs. stock abutments, there were no clear tendencies; some clones had lower levels of micromotion than the stock abutments, and others had higher levels. The clear message is that the implant-abutment relationship is system/manufacturer-specific. While this article is a thorough read, it is clinically relevant if you work with any of the evaluated systems. Prosthetic food for thought included the significantly less micromotion found in cast-to abutments compared to copy-milled and stock abutments, and engaged abutments (abutments with an anti-rotational feature) compared to nonengaging abutments (Figures 1 and 2).
The second thing I want to highlight is a systematic review and meta-analysis, completed by Torrecillas-Martinez et al., looking at implant-supported fixed partial dentures with cantilevers that extended less than 15 mm, and a possible correlation with marginal bone loss (MBL) and/or prosthetic complications in humans. Cantilevers are not recommended in tooth-supported prostheses due to the rotational occlusal forces that jeopardize the abutment teeth. This same potential compromise is also a concern with cantilevers and abutment dental implants. In this study, the follow-up times were between three and eight years with an overall MBL ranging from 0.36 to 1.08 mm, and a mean of 0.72 mm with no significant difference found in regard to MBL between implant-supported fixed prostheses with and without cantilevers. This was also the trend with porcelain fractures, being the most common implant-supported fixed prostheses complication with or without cantilevers (reported up to 39.2%). Abutment screw loosening was found to be higher for the prostheses with cantilevers. Clinical considerations when an implant-supported cantilever is being proposed would include utilizing more than one implant to support the cantilever and splinting all of the restorations together. It is proposed that complications are common independent of the presence of a cantilever due to other factors such as bruxism, heavy occlusal forces, and/or overloading.
ADDITIONAL READING |SRR 'Spotlight on JOMI': Recent issue of JOMI paves the way for future dental implant thinking
The final thing I want to highlight is the fact that several techniques and philosophies exist for maintaining the esthetics when an anterior tooth is deemed hopeless. In this issue, Siormpas et al. reported success and crestal bone loss data from 46 patients with a mean follow-up time of around three years on a “Root-Membrane” technique utilizing no bone graft and/or other biomaterials. The authors propose that by leaving the buccal aspect of the root at the time of immediate implant placement, the esthetics will be preserved. A flapless approach is used with immediate temporization of the dental implant. The success rate was determined clinically and radiographically, and found to be 97% comparable to conventional immediate implant placement. Mean crestal bone loss was 0.18 mm at the mesial and 0.21 mm at the distal. Authors attribute their success to a strict exclusion criterion. CBCT images were taken in four patients, revealing a radiolucent line delineating the implant-root interface. No human histology was presented to determine what was actually present between the root and implant. I would expect an overall good result since the technique includes an atraumatic surgical technique with immediate temporization. It cannot be concluded that this technique had better esthetics given there is not a control to serve as a comparison, nor were initial and final esthetic clinical parameters reported.
ADDITIONAL READING |AO 2015 annual meeting keynote preview: Dr. Daniel Alam focuses on the power of collaboration and the team approach in health care
The diversity of the topics covered above is a true reflection of the AO members themselves. What’s unique about AO is that it brings dentists, prosthodontists, periodontists, oral surgeons, lab technicians, and allied staff together — from around the world — at one meeting to discuss all facets of dental implant therapy. We are busy finalizing arrangements for AO’s 2015 Annual Meeting and our YCC Reception. This year’s YCC Reception will be at the trendy 111 Minna Gallery in San Francisco. It’s a great way to start the meeting and converse with colleagues from around the world. I attended my first AO meeting on my own, fresh out of residency with few financial resources, and it more than paid off. Today, with a busy practice and twin toddlers at home, attending remains a priority for me. Simply put, the AO Annual Meeting makes me a better surgeon.
One of the many benefits of being an AO member is an automatic JOMI (bimonthly) subscription.