Have any of your patients walked in, lifted their lip, and said, “Look, Doc, I am really getting long in the tooth, and it is sensitive too!” Well, here are some facts you can share with them. They are not alone; some 88% of individuals 65 years of age and older, and approximately 50% of individuals 18–64 years of age experience gingival recession at one or more tooth sites. (1,2)
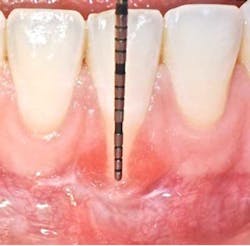
Gingival recession is defined as “the migration of the marginal soft tissue apical to the cementoenamel junction” (CEJ). Histologically, the destruction is associated with the loss of periodontal connective tissue fibers and alveolar bone, leading to exposure of the root surface to the oral environment. (3)This loss of hard- and soft-tissue-supporting structures ultimately increases the probability that patients will experience thermal or tactile sensitivity, esthetic concerns, and an increased susceptibility for root caries.
ALSO BY DR. DOOBROW |Biomimetic technology: putting the tooth fairy out of business
Ideally, surgical treatment of gingival recession defects should completely restore the anatomy of the mucogingival complex. This implies the regeneration of the attachment apparatus of the tooth, including the cementum with functionally oriented connective tissue fibers, periodontal ligament, and alveolar bone. It also infers the re-creation of topographic relations between the keratinized tissue and the alveolar mucosa that are functionally and esthetically acceptable to the patient. (3)
According to the proceedings from the 2014 American Academy of Periodontology Regeneration Workshop, root coverage may be attained through the application of a variety of surgical procedures. These outcomes are generally measured by reduced defect depth, gain in clinical attachment, and an increase in keratinized tissue. The associated systematic reviewprovides clear evidence that a subepithelial connective tissue graft (SCTG) procedure offers the best outcome for mean and complete root coverage, as well as an increase in keratinized tissue. (4,5) Strong evidence also supports biomaterials such as acelullar dermal matrix grafts (ADMG) or enamel matrix derivative (EMD) in conjunction with a coronally advanced flap (CAF) that can be used as an alternative to treat Miller Class I and II single-tooth gingival recession defects (figures 1 and 2). (6)Another suggestion from the proceedings was that using a split-thickness flap or tunnel technique can help to revascularize the graft by maintaining an excellent vascular supply to the flap.
ALSO BY DR. DOOBROW |Retirement planning for dentists: Investing today for a better tomorrow
Depending on the severity and extent that the mucogingival defects present, we often administer a hybrid/combination therapy. Many of our patients previously experienced mucogingival grafting procedures at other offices, searched the Internet, or discussed with friends who have had soft-tissue grafts, and as a result they are extremely fearful of the dreadful “pizza burn” that one may experience after harvesting from the palate. As reported in the literature and confirmed clinically in our office, with the addition of an enamel matrix protein, patients consistently report minimal postoperative swelling and discomfort. This has been a huge game changer for our practice and will be for yours too (figure 3). (7)
There is certainly no panacea for treatment, but we have found this combination therapy provides our patients with long-term predictable, stable results. Our preferred treatment method for gingival recession defects affecting one to four teeth is to use a tunneling technique in combination with a subepithelial connective tissue graft, enamel matrix derivative, and a coronally advanced flap (figures 4-9). When treating four or more teeth, or if a patient is opposed to harvesting a SCTG, we use a tunneling procedure in conjunction with an acellular dermal matrix graft, enamel matrix derivative, and a coronally advanced flap.
The addition of a biologic agent, specifically enamel matrix derivative, and our combination therapy has allowed us to minimize previously experienced discomfort at the graft site and predictably treat problems affecting more than 50% of our adult patients. Now it is your turn to eliminate those “long in the tooth” problems and recession-proof your practice!
References
1. Miller AJ, Brunelle JA, Carolos JP, Brown LJ, Loe H. Oral Health of United States Adults. The National Survey of Oral Health in US Employed Adults and Seniors: 1985–1986. (NIH Publication No. 87-2868).
2. Albandar JM, Kingman A. Gingival recession, gingival bleeding, and dental calculus in adults 30 years of age and older in the United States, 1988–1994. Journal of Periodontology. 1999;70(1):30-43.
3. Trombelli L. Periodontal regeneration in gingival recession defects. Periodontol 2000. 1999;19:138-150.
4. Richardson CR, Allen EP, Chambrone L, Langer B, McGuire MK, Zabalequie I, Zade HH, Tatakis DN. Periodontal soft tissue root coverage procedures: Practical applications from the AAP Regeneration Workshop. Clin Adv Periodontics. 2015;5:2-10.
5. Tatakis DN, Chambrone L, Allen EP et al. Periodontal soft tissue root coverage procedures: A consensus report from the AAP Regeneration Workshop. J Periodontol. 2015;86(Suppl. 2):S52-S55.
6. Miller PD Jr. A classification of marginal tissue recession. Int. J. Periodontics Restorative Dent. 1985;5(2):8-13.
7. Jepson M, et al. J Periodontol. Aug. 2004;75(8):1150.