The main goal when restoring health, function, and esthetics of lost tissue due to gingival recession is to accomplish surgery the most efficiently with the fewest postoperative complications. This article briefly reviews the history of noninvasive soft-tissue grafting and describes a new surgical protocol—the Pinhole Surgical Technique—that has taken soft-tissue grafting awareness to a new level.
WHEN EVALUATING THE FACTORS THAT CONTRIBUTE TO SMILE ESTHETICS,harmony, balance, and continuity of form must be considered. Gingival architecture forms the foundation for the emergence of the tooth, and when gingival recession is present, the properties of smile esthetics can be tarnished. Gingival grafting (gum grafting) is an umbrella term encompassing many different surgical techniques that can be used to correct gum recession.
The main goal when restoring health, function, and esthetics of lost soft tissue is to accomplish the surgery in the most efficient manner with the fewest postoperative complications. To achieve this end goal, minimally invasive soft-tissue grafting protocols were created and continue to advance. This article will briefly review the history of noninvasive soft-tissue grafting and describe a new surgical protocol—the Pinhole Surgical Technique (PST)—that has taken soft-tissue grafting awareness to a new level.
Development of early surgical tissue-grafting techniques
One of the first surgical techniques proposed to cover gingival recession and increase keratinized tissue was the free gingival graft. (1) Although this technique is very effective, it requires a second surgical site, the color match between the graft and recipient site is not ideal, and postoperative discomfort can be extreme.
An advance in palatal grafting came in the form of the subepithelial connective tissue graft (CTG) as color match was ideal and postoperative discomfort decreased. (2) This technique still requires a secondary site, however, vertical incisions to advance the flap over the graft tissue, and donor site morbidity. The next advancements in noninvasive soft-tissue grafting attempted to eliminate the need for vertical incisions with envelope incisions (3) and semilunar incisions. (4)
Eventually these minimally invasive techniques, used to treat one or two areas of adjacent recession, gave rise to "tunnel" techniques, which were used to treat multiple areas of recession on contiguous teeth. (5) This type of soft-tissue grafting uses small incisions made in the mucosa and elevation of the tissue without traditional mucoperiosteal reflection (figure 1). By eliminating vertical incisions and the need for reflecting the papilla, postoperative discomfort decreased and surgically induced tissue recession was minimized. (6)
Further advances were made as the need to harvest gum tissue from the palatal region became obsolete when this tunnel technique was combined with allograft (human) or xenograft (animal) soft tissue, further minimizing postoperative discomfort without reducing the efficacy of the graft coverage. (7) Once these surgical protocols had been refined, the next step in minimally invasive soft-tissue grafting was to create specialized instruments specific to tunneling procedures that facilitated surgical reconstruction of gingival defects. (8)
The Pinhole Surgical Technique
The Pinhole Surgical Technique (PST) is another example of a recent advancement in minimally invasive soft-tissue grafting surgery that combines specialized surgical instrumentation and a modification of the tunnel technique. The PST is a modified tunnel technique that utilizes "pinhole" incisions made in the alveolar mucosa with a syringe needle. The number of these pinhole incisions made is determined by the number of teeth that need to be treated, and the incisions are placed 6-7 mm above the mucogingival junction (figures 2 and 2a).
Specialized instruments are then used to elevate the mucoperiosteal envelope of tissue that can be coronally advanced from the original tissue level to 3-5 mm above the desired level of tissue coverage (figures 3 and 3a). Root surfaces of the teeth to be treated are mechanically debrided and, in some cases, chemically modified (this is the author’s protocol, not the original protocol) to remove accretions and smear layer. After sufficient tissue release, noncross-linked collagen membrane strips are placed into the pinhole incisions as a means of providing tissue bulk and support (figure 4). Some clinicians have begun to use platelet-rich fibrin membranes instead of or in addition to collagen membranes, but this is a deviation from traditional protocol (figure 5). After enough regenerative material is placed and the envelope of tissue has been sufficiently bulked and advanced, the procedure is finished.
Original PST protocol does not advocate the need for suturing the tissue flaps. The thought is that the clotting process alone will keep the tissue at the desired advanced level. Once again, some clinicians deviate from this protocol and use sling sutures to ensure that the tissue stays coronally positioned.
Standards, studies, and statistics
Using the PST protocol, one study measured 85 recession sites that were Miller Class I or Class II recession with a mean follow-up time of one-and-a-half years. Defect coverage was obtained in 91% of the cases and near-complete root coverage in 81% of the cases. Clinical attachment gain was 4.4 mm, and keratinized tissue gain was 1.4 mm. (9) Additionally, some of the biggest advantages of this technique are in the subjective patient assessment realm. Time of the surgical procedure compared to conventional soft-tissue grafting techniques was decreased. Postoperative patient discomfort and swelling were also extremely reduced.
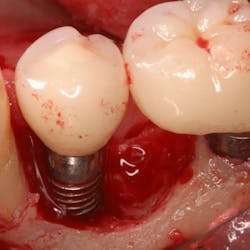
When Miller Class III recessions were included, complete root coverage dropped to 69%, and 90% root coverage was obtained in 77% of the cases. Therefore, PST has been indicated as an appropriate soft-tissue grafting technique around natural teeth with two or more areas of recession in the Miller Class I and Class II ranges. This method is currently being explored around dental implants with soft-tissue loss, but as of today, there are no studies in the literature to prove this is effective.
Improving case acceptance and awareness
Advances in minimally invasive soft-tissue grafting techniques over the years have improved case acceptance, while decreasing postoperative pain and complications of traditional gum grafting surgery. PST is an example of another surgical advancement that has furthered patient acceptance and awareness of the benefits of gum grafting. Grassroots effort and media publications of the PST have augmented the general public’s knowledge about the benefits of soft-tissue grafting and have taken a once-ominous procedure and made it more palatable.
References
1. Aichelmann-Reidy ME, Yukna RA, Evans GH, Nasr HF, Mayer ET. Clinical evaluation of acellular allograft dermis for the treatment of human gingival recession. J Periodontol. 2001;72(8):998-1005.
2. Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985;56(12):715-720.
3. Raetzke PB. Covering localized areas of root exposure employing the “envelope” technique. J Periodontol. 1985;56(7): 397-402.
4. Tarnow DP. Semilunar coronally repositioned flap. J Clin Periodontol. 1986;13(3):182-185.
5. Zabalegui I, Sicilia A, Cambra J, Gil J, Sanz M. Treatment of multiple adjacent gingival recessions with the tunnel subepithelial connective tissue graft: a clinical report. Int J Periodontics Restorative Dent. 1999;19(2):199-206.
6. Allen AL. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. I. Rationale and technique. Int J Periodontics Restorative Dent. 1994;14(3):216-227.
7. Andrade PF, Felipe ME, Novaes AB Jr, et al. Comparison between two surgical techniques for root coverage with an acellular dermal matrix graft. J Clin Periodontol. 2008;35(3):263-269. doi: 10.1111/j.1600-051X.2007.01193.x.
8. Zuhr O, Fickl S, Wachtel H, Bolz W, Hürzeler MB. Covering of gingival recessions with a modified microsurgical tunnel technique: case report. Int J Periodontics Restorative Dent. 2007;27(5):457-463.
9. Chao JC. A novel approach to root coverage: the pinhole surgical technique. Int J Periodontics Restorative Dent. 2012;32(5):521-531.