Opioid alternative non-narcotic dosing: By the clock
Editor’s note: Originally published December 16, 2014. Updated for clinical accuracy December 1, 2022.
The problem
Data from the Centers for Disease Control and Prevention (CDC) show more than 93,000 individuals in the United States died from a drug overdose in 2020, a 29.4% increase from the previous year. Of those deaths, 69,710 involved opioids. In 2021, an estimated 107,622 deaths from drug overdose occurred, a 15% increase over the previous record of 93,655 set in 2020. Drug overdose deaths rose 30% from 2019 to 2020. Opioid addiction is so prevalent in the US that it has reached epidemic proportions and prompted the CDC in 2022 to revise its 2016 opioid guidelines, making them more stringent in favoring non-narcotic analgesics over their narcotic counterparts.1
Dental pain: Can we predict who has a higher risk prior to treatment?
Street drugs: Even more dangerous than before
By the clock
Efficacy and safety of nonnarcotic drug therapy for the management of mild to acute postoperative pain typically involves orally administered analgesics such as ibuprofen, naproxen, acetaminophen, and tramadol. The literature has shown similar therapeutic efficacy when using a combination therapy of ibuprofen and acetaminophen (I-P) as compared with narcotic counterparts. I-P therapy can be more effective with fewer side effects than narcotics if prescribed correctly. Most clinicians will prescribe analgesics in an “as needed for pain” (PRN) manner. But there is a better way than PRN, and that is by the clock.
Rather than wait for pain to spike, the by-the-clock approach instructs patients to take their medications at a preappointed time. This method does not wait for pain to arrive, as once pain presents, it can be very difficult to get the patient comfortable again (up to a few days). In addition, patients experiencing severe, unrelenting pain may take more pain medication, which is not without consequences. Overdose, nausea, constipation, respiratory depression, etc., are all sequelae that can result from overmedicating.
The by-the-clock postsurgical pain protocol is very effective when using a combination of ibuprofen and acetaminophen, which addresses both the intrinsic and extrinsic inflammatory pathways. Acetaminophen and ibuprofen do just that—attack and control both pathways if monitored prior to the onset of pain and in a regulated manner.
Presurgical protocol
- 600 mg of Advil the night before surgery.
- 600 mg of Advil the morning of the surgery. If the patient has been instructed to take nothing by mouth (NPO) eight hours prior to the surgery, it is acceptable to make an exception for medication with a little water.
Postsurgical protocol
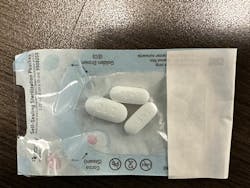
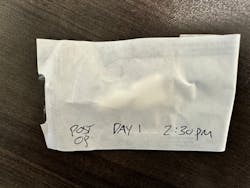
Envelopes are prepared with two Advil and one 500 mg Tylenol (figure 1). Start with the first dose in the office after the procedure. On each of the envelopes (figure 2), we boldly mark the time that patients need to swallow the contents, even if that means waking up in the middle of the night. The perfect time to maximize the pain control is every four hours. Years ago, I would ask patients to follow my OTC by-the-clock regimen with varying results. Not until I dispensed the medication chairside with the premade pill packets did I realize the true potential of this method. It’s extremely important to get off on the right foot with this protocol. Patient compliance can be sketchy. However, we have seen dramatic improvement in compliance with the envelopes we give each of our surgery patients. I’ve become a real fan of this protocol.
If your patient’s procedure is a big one—i.e., bilateral sinus augmentations with a bunch of implants—I would supply envelopes with pain meds for two or three days. Start with 800 mg of ibuprofen and 1,000 mg of acetaminophen. For less invasive procedures, I would recommend one day of pain medication or one day’s worth of envelopes. After the one or two days are complete, I would advise the PRN approach. Different protocols would need to be used with your kidney- or liver-compromised patients.
RICE therapy
In addition to the by-the-clock pain control protocol, we have one adjunctive therapy with the acronym of R.I.C.E.: rest, ice, compression, and elevation. As dentists, we typically do not use cryotherapy to its full advantage. In my practice, we advocate 24 hours of nonstop compressive ice packs over the surgical site for the first day, with four additional hours of compressive ice on the second day—20 minutes on and 20 minutes off with the ice. Elevation refers to the surgical site position relative to the patient’s heart. We request that our patients sleep with two pillows or even in a La-Z-Boy lounge chair to help with this elevation.
We hope this info is helpful for your surgical outcomes. Give it a try. It has been a solid addition to postoperative pain control for our patients.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
Reference
- Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC clinical practice guideline for prescribing opioids for pain – United States, 2022. MMWR Recomm Rep. 2022;71(No. RR-3):1-95. doi:10.15585/mmwr.rr7103a1
P.K. Clark, DMD, is a practicing dentist, lecturer, and surgical mentor. He is a graduate of Oregon Health and Science University and maintains private practices in Portland, Oregon, and Heber City, Utah. Dr. Clark founded the unique WhiteCap Institute, which allows him to spend time building relationships and teaching on subjects he is most passionate about. He is an active member in various dental societies including the International Congress of Oral Implantology, the American Academy of Implant Dentistry, the Academy of General Dentistry, and the American Dental Association.
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a PhD candidate in the field of functional and integrative nutrition. Contact him through his website at drscottfroum.com or (212) 751-8530.
P.K. Clark, DMD
P.K. Clark, DMD, is a practicing dentist, lecturer, and surgical mentor. He is a graduate of Oregon Health and Science University and maintains private practices in Portland, Oregon, and Heber City, Utah. Dr. Clark founded the unique WhiteCap Institute, which allows him to spend time building relationships and teaching on subjects he is most passionate about. He is an active member in various dental societies including the International Congress of Oral Implantology, the American Academy of Implant Dentistry, the Academy of General Dentistry, and the American Dental Association.