Originally published in 2017. Updated in 2022.
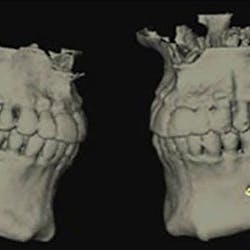
The gummy smile is caused by gingival enlargement and can be induced by three main causes: (1) inflammation, (2) medication, and (3) systemic disease. Treatment can be in the form of natural healing, once the etiology is removed, by instituting proper dental hygiene, and through nonsurgical treatment and/or surgical treatment.
This article will briefly discuss examples of gingival enlargement and its associated causes, as well as present surgical treatment that can assist in correcting certain types of gingival enlargement.How does oral bacteria cause gingival enlargement?
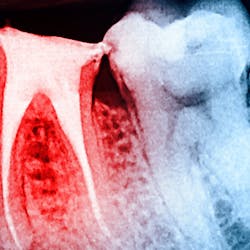
One reason people develop gummy smiles is inflammatory-induced gingival enlargement, typically caused by biofilm (bacteria) and the host response. Gum disease (gingivitis and periodontitis) can result in gum tissue swelling, redness, gum overgrowth, and bleeding (figure 1). In addition to bacterial infiltration of the gums due to poor oral hygiene, orthodontic appliances have been associated with gingival enlargement since braces can act as food traps (figure 2).Further reading: Considerations when using veneers to fabricate a perfect smile
Medications that cause gingival enlargement
Medication-induced (drug-induced) gingival enlargement can be caused by certain classes of drugs people may be taking.1 The following classes of drugs have been associated with gum overgrowth:
- Anticonvulsants (phenytoin, phenobarbital, lamotrigine, vigabatrin, ethosuximide, topiramate, and primidone)
- Antihypertensives (calcium channel blockers such as nifedipine, amlodipine, and verapamil)
- Immunosuppressants (cyclosporine)
- Amphetamines (cocaine, Ritalin, methamphetamine)
- 50% of the cases are typically attributed to phenytoin (figure 3).
- 30% of the cases are typically attributed to cyclosporine.
- 10% to 20% of the cases are typically attributed to calcium channel blockers, with nifedipine being the most notable problem (figures 4a and 4b).
- 10% or fewer of the cases are typically attributed to amphetamines.
What are the systemic causes of gingival enlargement?
Systemic causes of gingival enlargement may result in localized gum tissue overgrowth or a generalized response in which all the teeth are affected. Consider these systemic causes:
- Hormonal changes associated with pregnancy or puberty
- Diseases requiring hormone replacement therapy
- Vitamin deficiencies (mostly vitamin C and vitamin Bs)
- Benign neoplasms such as giant cell granuloma, papillomas, and fibromas
- Other more serious causes of gingival enlargement include leukemias, malignant neoplasms/carcinomas, as well as many forms of granulomatous diseases.
Treatment of gingival enlargement
If these methods are ineffective, surgical treatment is warranted. Conventional surgical treatment includes the use of surgical blades, knives, and high-speed burs to remove the excess gingival tissue. Dental lasers such as diodes, 10.6 micron CO2, erbium YAG, erbium chromium YAG, and Nd:YAG lasers have also been implemented to remove excess soft tissue.3
Another laser that has been used to treat gingival enlargement and gummy smiles is a 9.3 micron CO2 laser (Solea from Convergent Dental; figure 2a). Unlike other lasers, the Solea laser has the capabilities of removing both soft and hard tissue, precise cutting accuracy due to control of both laser beam power and size, and the ability to cauterize inflamed tissue (figures 4c and 4d). Conventional instrumentation—such as blades, knives, and high-speed burs—can often lead to bleeding after surgical removal when the tissue is inflamed. With this type of CO2 laser, sutures and/or surgical dressing are often not needed.
Conclusion
Treatment of the gummy smile due to gingival enlargement is dependent on the etiologic agent and the category the disease falls under. If the enlargement is induced by medication, suspension of the drug and institution of proper home care will resolve the problem. When caused by a systemic problem, treatment of the disease usually will result in treatment of the gingival enlargement. Hormonal fluctuations caused by pregnancy and puberty are often unavoidable; many times, gingival enlargement can be precluded/alleviated with excellent home care and routine dental maintenance visits. When these noninvasive modalities do not result in a resolution of the gingival enlargement, surgical treatment is often needed to remove excess tissue.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
References
- Tungare S, Paranjpe AG. Drug-induced gingival overgrowth. [Updated 2021 Sep 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538518/
- Kim JY, Park SH, Cho KS, et al. Mechanism of azithromycin treatment on gingival overgrowth. J Dent Res. 2008;87(11):1075-1079. doi:10.1177/154405910808701110
- Lione R, Pavoni C, Noviello A, Clementini M, Danesi C, Cozza P. Conventional versus laser gingivectomy in the management of gingival enlargement during orthodontic treatment: a randomized controlled trial. Eur J Orthod. 2020;42(1):78-85. doi:10.1093/ejo/cjz032