The ideal outcome of dental and periodontal care is to maintain the health, comfort, function, and esthetics of the natural dentition.1 When destruction is associated with the loss of periodontal connective tissue fibers and alveolar bone, exposure of the root surface to the oral environment will occur, resulting in gingival recession. Gingival recession (GR) is defined as the migration of the marginal soft tissue apical to the cementoenamel junction (CEJ).2 This loss of hard- and soft-tissue-supporting structures ultimately increases the probability that patients will experience soft-tissue discomfort, thermal or tactile sensitivity, esthetic concerns, an interference with the performance of adequate plaque control, as well as an increase in susceptibility for root caries and overall inflammatory insult. Gingival recession at one or more tooth sites is extremely common, affecting 50% of individuals ages 18–64 and 88% of those age 65 and older.2,3
Keratinized tissue (KT) is the part of the oral mucosa that covers the gingiva and hard palate. It extends from the free gingival margin to the mucogingival junction and consists of the free gingiva and the attached gingiva. The band of keratinized tissue around natural dentition and implants is vital in maintaining oral health, preventing periodontal recession, and maintaining overall esthetics.4,5 KT can provide increased resistance of the periodontium to external injury, contribute to the stabilization of the gingival margin position, and aid in the dissipation of physiological forces exerted by the muscular fibers of the alveolar mucosa and the gingival tissues.6
The importance of the presence of keratinized tissue remains controversial. Various studies have shown that lack of keratinized soft tissue around teeth and implants can have negative consequences in both function and esthetics. Prospective and retrospective studies have shown that in the presence of suboptimal plaque control and clinical inflammation, attachment loss and gingival recession may result unless a minimum amount of 2 mm of keratinized and attached tissue are present. On the contrary, it has been reported that a minimum of KT is not needed to prevent attachment loss when optimal plaque control is present.4,5,7
It is imperative to effectively communicate the importance of attached and keratinized tissue to patients. Utilizing an analogy that patients can comprehend will be beneficial and aid in treatment acceptance, and it will ultimately help the patient maintain the health, comfort, function, and esthetics of the natural dentition and/or integrity of dental implants. One supportive analogy would be to compare keratinized and attached tissue to a cuff on a long-sleeved shirt or jacket. With this visual, the tighter the sleeve cuff, the more protection the teeth and/or implants will have.
Treatment of mucogingival deformities—specifically gingival recession—requires gingival augmentation procedures that address both a functional and esthetic component for the patient. These procedures were first introduced in the 1960s.8,9
Ideally, surgical treatment of gingival recession defects should completely restore the anatomy of the mucogingival complex. This implies the regeneration of the attachment apparatus of the tooth, including the cementum with functionally oriented connective tissue fibers, periodontal ligament, and alveolar bone, as well as the re-creation of topographic relations between the keratinized tissue and the alveolar mucosa that are functionally and esthetically acceptable to the patient.10
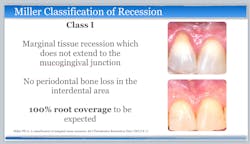
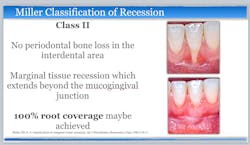
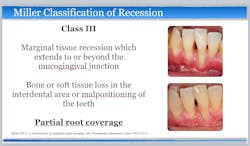
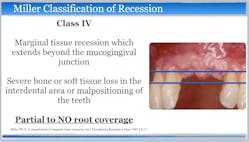
Current evidence regarding the treatment of gingival recession defects indicates that surgical therapeutic approaches are highly predictable for Miller class I and II single-tooth defects.1,11,12 A number of systematic reviews and randomized clinical trials have demonstrated the successful use of subepithelial connective tissue graft (SCTG) techniques when treating maxillofacial Miller class I and II single-tooth defects (figures 1 and 2). However, surgical challenges arise when patients present with Miller class III and IV defects, as well as multiple-tooth GR defects and linguopalatal mucogingival concerns (figures 3 and 4).1,11
In conclusion, with proper patient selection and education—as well as excellent surgical execution and optimal plaque control—significant long-term functional, esthetic, and periodontal health can be maintained.
References
- Richardson CR, Allen EP, Chambrone L, Langer B, McGuire MK, Zabalegui I, Zadeh HH, Tatakis DM. Periodontal soft tissue root coverage procedures: practical applications from the AAP Regeneration Workshop. Clin Adv Periodontics. 2015;5(1):2-10. doi:10.1902/cap.2015.140059
- Albandar JM, Kingman A. Gingival recession, gingival bleeding, and dental calculus in adults 30 years of age and older in the United States, 1988–1994. J Periodontol. 1999;70(1):30-43. doi:10.1902/jop.1999.70.1.30
- National Institute of Dental Research (U.S.). 1987. Oral health of United States adults: the National Survey of Oral Health in U.S. Employed Adults and Seniors, 1985-1986. NIH Publication no. 87-2868. U.S. Dept. of Health and Human Services, Public Service, National Institutes of Health; 1987.
- Schrott AR, Jimenez M, Hwang J-W, Fiorellini J, Weber H-P. Five-year evaluation of the influence of keratinized mucosa on peri-implant soft-tissue health and stability around implants supporting full-arch mandibular fixed prostheses. Clin Oral Implants Res. 2009;20(10):1170-1177. doi:10.1111/j.1600-0501.2009.01795.x
- Chung DM, Oh T-J, Shotwell JL, Misch CE, Wang H-L. Significance of keratinized mucosa in maintenance of dental implants with different surfaces. J Periodontol. 2006;77(8):1410-1420. doi:10.1902/jop.2006.050393
- Lang NP, Löe H. The relationship between the width of keratinized gingiva and gingival health. J Periodontol. 1972;43(10):623-627. doi:10.1902/jop.1972.43.10.623
- Souza AB, Tormena M, Matarazzo F, Araújo MG. The influence of peri-implant keratinized mucosa on brushing discomfort and peri-implant tissue health. Clin Oral Implants Res. 2016;27(6):650-655. doi:10.1111/clr.12703
- Sullivan HC, Atkins JH. Free autogenous gingival grafts. I. Principles of successful grafting. Periodontics. 1968;6(3):121-129.
- Sullivan HC, Atkins JH. Free autogenous gingival grafts. 3. Utilization of grafts in the treatment of gingival recession. Periodontics. 1968;6(4):152-160.
- Trombelli L. Periodontal regeneration in gingival recession defects. Periodontol 2000. 1999;19(1):138-150. doi:10.1111/j.1600-0757.1999.tb00152.x
- Chambrone L, Tatakis DN. Periodontal soft tissue root coverage procedures: a systematic review from the AAP Regeneration Workshop. J Periodontol. 2015;86(25 Suppl 2):S8-S51. doi:10.1902/jop.2015.130674
- Tatakis DN, Chambrone L, Allen EP, et al. Periodontal soft tissue root coverage procedures: a consensus report from the AAP Regeneration Workshop. J Periodontol. 2015;86 Suppl 2:S52-S55. doi:10.1902/jop.2015.140376
Related articles about saving teeth
- Saving teeth versus placing implants: A cost analysis
- Saving teeth with endodontic treatment: Lesion size and predictability of healing
- In the days of dental implants, why should we be keeping teeth?
Editor’s note: This article originally appeared in Perio-Implant Advisory, a newsletter for dentists and hygienists that focuses on periodontal- and implant-related issues. Perio-Implant Advisory is part of the Dental Economics and DentistryIQ network. To read more articles, visit perioimplantadvisory.com and subscribe at this link.