Saving teeth with endodontic treatment: Lesion size and predictability of healing
The vast majority of the dental community recognizes the importance and safety of root canals in saving the natural dentition. In the event natural teeth cannot be saved predictably with modern endodontics and properly restored, dental implants have been positioned as viable treatment options for replacing missing or extracted teeth. However, in its “Tooth Saving Tips” fact sheet, the American Association of Endodontists unequivocally states, “Saving a natural tooth through endodontic treatment should always be the first choice for the best health and cosmetic results.”1 It is imperative for any and all dental practitioners to provide evidence-based treatment options tailored to each unique patient experience with professional ethics and nonmaleficence steering the conversation.
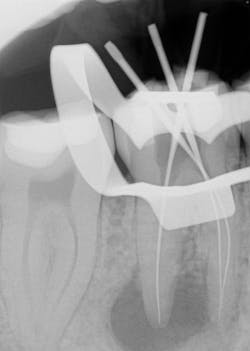
Various clinical presentations and risk factors can influence endodontic success or failure, including but not limited to the quality of the root canal performed and the seal of the coronal restoration.2 In addition to the aforementioned factors, the presence and size of a periapical lesion can directly affect the prognosis and treatment outcome. Classic literature highlights this shift in long-term success rates from 96% for vital/nonvital cases without the presence of a periapical lesion to 86% when a periapical lesion is present.3
Periapical radiographs have been commonly used to evaluate the size of periapical lesions. However, periapical radiographs have limitations, because the information is rendered in only two dimensions. A periapical lesion can only be detected in the radiograph when the mineral loss of bone reaches 30%–50%.4
Case presentation
Also by Dr. Marcus Johnson:
5 questions to ask when determining if teeth with perio-endo infections can be saved
Editor’s note: This article originally appeared in Perio-Implant Advisory, a newsletter for dentists and hygienists that focuses on periodontal- and implant-related issues. Perio-Implant Advisory is part of the Dental Economics and DentistryIQ network. To read more articles, visit perioimplantadvisory.com and subscribe at this link.
References
- Tooth saving Tips. AAE fact sheet. American Association of Endodontists. 2013. https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/toothsavingtips.pdf
- Ray HA, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J. 1995;28(1):12-18. doi:10.1111/j.1365-2591.1995.tb00150.x
- Sjogren U, Hagglund B, Sundqvist G, King W. Factors affecting the long-term results of endodontic treatment. J Endod. 1990;16(10):498-504. doi:10.1016/S0099-2399(07)80180-4
- Bender IB. Factors influencing the radiographic appearance of bony lesions. J Endod. 1997; 23(1):5-14. doi:10.1016/S0099-2399(97)80199-9
- Low KMT, Dula K, Bürgin W, von Arx T. Comparison of periapical radiography and limited cone-beam tomography in posterior maxillary teeth referred for apical surgery. J Endod. 2008;34(5):557-562. doi:10.1016/j.joen.2008.02.022
- Regezi JA. Periapical diseases: spectrum and differentiating features. J Calif Dent Assoc. 1999;27(4):285-289.
- Nair PNR, Pajarola G, Schroeder HE. Types and incidence of human periapical lesions obtained with extracted teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81(1):93-102. doi:10.1016/s1079-2104(96)80156-9
About the Author
Marcus Johnson, DDS, MSD
Marcus Johnson, DDS, MSD, is a graduate of Rutgers University and New York University Dental School. He received his Certificate of Endodontics from Case Western Reserve University, while concurrently earning his master’s degree in dentistry. Dr. Johnson, an astute evidence-based clinician and an active member of numerous dental organizations, won an award for his research on new treatment techniques. He is the lead attending endodontist for the general practice residency at Interfaith Medical Center in Brooklyn, New York, where he also teaches the pediatric residents. He is a member of the American Association of Endodontists’ board of directors, a diplomate of the American Board of Endodontics, and president of the New York State Association of Endodontists. As a board-certified endodontist, Dr. Johnson owns and operates City Endodontics, a private practice specializing in endodontics in Manhattan.