Saving teeth versus placing implants: A cost analysis
When analyzing the patient’s cost to maintain this treatment over a long period of time with hygiene intervals three to four times a year, dollar amounts range from $700 to $1,100 per year, again dependent upon geographic location. In a small subset of the population (less than 5% of patients with disease), refractory periodontal disease can still exist even with treatment. In such cases, treatment will have to be rendered continually to slow disease progression, increasing the overall costs of this type of therapy.6
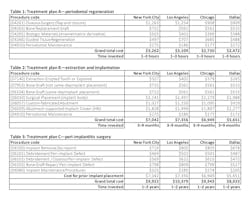
Tables 1–3 present actual treatment cost differences between the patient who opts to “save” the natural tooth (treatment plan A) and the one who chooses to “remove” the tooth via extraction and placement of an implant (treatment plan B). These fees vary according to geographic location and represent insurance codes from New York City, Los Angeles, Chicago, and Dallas.
Another scenario that took place in a private practice with actual dollar amounts can be seen in treatment plan C. This patient had already paid for treatment plan B in the $5,000–$7,000 range and subsequently presented to the practice with moderate peri-implantitis. In addition to the money the patient had already invested, she would now be responsible for the financial costs of treatment plan C.
After reviewing the additional costs and lengthy healing time involved with surgery to correct the ailing implant, the overall costs associated with treatment were in the $8,000–$10,000 range, with more than three years of treatment time invested. Of important note is that most insurance companies limit the amount of reimbursement for implant-related services. When dealing with insurance companies, accurate ADA coding and claims submission are critical to facilitate services and expedite reimbursement.
In conclusion, there are many factors to consider when deciding between saving the natural dentition and extracting and placing implants. All parties must consider the long-term economic impact on the patient as well as the long-term success rates of the treatment. Both implants and periodontal therapy to save natural teeth have high initial success rates, with implants usually incurring initial costs. However, when looking at long-term retention rates, natural teeth often demonstrate fewer complications and have a smaller financial impact when correction is needed.17
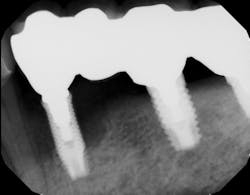
Author’s note: All photos courtesy of Scott Froum, DDS
Editor's note: Join us for the not-to-miss Perio-Implant Advisory Symposium on October 23, 2020. In this important virtual meeting, you’ll learn the newest skills it takes to save patients’ natural dentition. Bring your team and transform your practice. Conference schedule and special rates available at this link. Presented by Geistlich Biomaterials.
References
1. Howe MS, Keys W, Richards D. Long-term (10-year) dental implant survival: a systematic review and sensitivity meta-analysis. J Dent. 2019;84:9-21. doi:10.1016/j.jdent.2019.03.008
2. Levin L, Halperin-Sternfeld M. Tooth preservation or implant placement: a systematic review of long-term tooth and implant survival rates. J Am Dent Assoc. 2013;144(10):1119-1133. doi:10.14219/jada.archive.2013.0030
3. Setzer F, Kim S. Preserving the natural tooth versus extraction and implant placement: an evidence-based approach. Rosen E, Nemcovsky CE, Tsesis I, eds. In: Evidence-Based Decision Making in Dentistry. Springer International; 2017:73-95. https://doi.org/10.1007/978-3-319-45733-8
4. Axelsson P, Lindhe J, Nyström B. On the prevention of caries and periodontal disease. Results of a 15-year longitudinal study in adults. J Clin Periodontol. 1991;18(3):182-189. doi:10.1111/j.1600-051x.1991.tb01131.x
5. Hirschfeld L, Wasserman B. A long-term survey of tooth loss in 600 treated periodontal patients. J Periodontol. 1978;4(5):225-237. doi:10.1902/jop.1978.49.5.225
6. Magnusson I, Walker CB. Refractory periodontitis or recurrence of disease. J Clin Periodontol. 1996;23(3):289-292. doi:10.1111/j.1600-051x.1996.tb02091.x
7. Simonis P, Dufour T, Tenenbaum H. Long-term implant survival and success: A 10-16-year follow-up of non-submerged dental implants. Clin Oral Implants Res. 2010;21(7):772-777. doi:10.1111/j.1600-0501.2010.01912.x
8. Schwendicke F, Graetz C, Stolpe M, Dörfer CE. Retaining or replacing molars with furcation involvement: a cost-effectiveness comparison of different strategies. J Clin Periodontol. 2014;41(11):1090-1097. doi:10.1111/jcpe.12315
9. Øystein F, Grytten J. A comparison of teeth and implants during maintenance therapy in terms of the number of disease‐free years and costs—an in vivo internal control study. J Clin Periodontol. 2013;40(6):645-651. doi:10.1111/jcpe.12101
10. Froum SJ, Froum SH, Rosen P. A regenerative approach to the successful treatment of peri-implantitis: a consecutive series of 170 implants in 100 patients with 2- to 10-year follow-up. Int J Periodontics Restorative Dent. 2015;35(6):857-863. doi:10.11607/prd.2571
11. Lindhe J, Meyle J, Group D of European Workshop on Periodontology. Peri-implant diseases: consensus report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008;35(suppl 8):282-285. doi:10.1111/j.1600-051X.2008.01283.x
12. Salvi GE, Persson GR, Heitz-Mayfield LJA, Frei M, Lang NP. Adjunctive local antibiotic therapy in the treatment of peri-implantitis II: clinical and radiographic outcomes. Clin Oral Implants Res. 2007;18(3):281-285. doi:10.1111/j.1600-0501.2007.01377.x
13. Froum SJ, Froum SH, Rosen PS. Successful management of peri-implantitis with a regenerative approach: a consecutive series of 51 treated implants with a 3- to 7.5- year follow-up. Int J Periodontics Restorative Dent. 2012;32(1):11-20.
14. Froum S. Top 5 anatomical differences between dental implants and teeth that influence treatment outcomes. Perio-Implant Advisory. September 12, 2017. https://www.perioimplantadvisory.com/clinical-tips/periodontal-complications/article/16412223/top-5-anatomical-differences-between-dental-implants-and-teeth-that-influence-treatment-outcomes
15. Heitz‐Mayfield LJA, Salvi GE, Mombelli A, et al. Supportive peri‐implant therapy following anti‐infective surgical peri‐implantitis treatment: 5‐year survival and success. Clin Oral Implants Res. 2018;29(1):1-6. doi:10.1111/clr.12910
16. Pretzl B, Wiedemann D, Cosgarea R, et al. Effort and costs of tooth preservation in supportive periodontal treatment in a German population. J Clin Periodontol. 2009;36(8):669-676. doi:10.1111/j.1600-051X.2009.01409.x
17. Donos N, Laurell L, Mardas N. Hierarchical decisions on teeth vs. implants in the periodontitis‐susceptible patient: the modern dilemma. Periodontol 2000. 2012;59(1):89-110. doi:10.1111/j.1600-0757.2011.00433.x
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of the American Board of Periodontology, is a clinical associate professor at SUNY Stony Brook School of Dental Medicine in the Department of Periodontology. He serves on the board of editorial consultants for the Academy of Osseointegration's Academy News. Contact him through his website at drscottfroum.com or (212) 751-8530.
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.

Kyle Summerford
Kyle Summerford is a leader in dental office management. Over the course of 18 years, he has established himself as a self-proclaimed financial guru. He is founder and president of Summerford Solutions Inc. and cofounder of elitedentalclaims.com, which is aimed at helping dental practices across the US overcome their challenges with navigating dental insurance plans. Summerford is a dynamic lecturer and author. He serves as editorial director of DentistryIQ’s Dental Office Manager Digest newsletter. His monthly column, Coding with Kyle, is a terrific source of information for dental professionals.