Clinical applications for the 2018 classification of peri-implant diseases and conditions
Susan Wingrove, BS, RDH, focuses on the clinical applications of peri-implant diseasesand conditions in light of the AAP/EFP's new 2018 classification. This information will make it easier to assess your patients' periodontal status, as well as monitor their oral health and condition of their implants to ensure long-term success.
THEAMERICAN ACADEMY of Periodontology (AAP) and European Federation of Periodontology (EFP) met in November 2017. Their efforts resulted in the Proceedings of the World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions, which was published in 19 review papers and four consensus reports. For more detailed information regarding changes to disease classification, refer to the full proceedings of the World Workshop of the AAP and EFP. (1)
The focus of this article is on the understanding and clinical applications of peri-implant diseases and conditions. This information will make it easier to assess the periodontal status of your patients, as well as monitor their oral health and the condition of their dental implants to ensure success over the long term. For the periodontal disease summary, please see "The new classification of periodontal disease that you, your patient, and your insurance company can understand," by Scott Froum, DDS, editorial director of Perio-Implant Advisory, published August 30, 2018.
The peri-implant disease classification is similar to the stages and grading for periodontal disease with its four major categories: peri-implant health, peri-implant mucositis, peri-implantitis, and peri-implant soft- and hard-tissue deficiencies (table 1). (1)
Table 1: Categories of peri-implant diseases and conditions
1. Peri-implant health—the absence of erythema (inflammation), bleeding on probing (BOP), swelling, and suppuration with no bone loss (BL) < 2.0 mm
2. Peri-implant mucositis—inflammation, presence of BOP, swelling, no BL < 2.0 mm, and strong evidence that plaque (biofilm) is the etiologic factor
3. Peri-implantitis—inflammation, plaque-associated pathological condition in tissue, probing depth (PD) ≥ 4–8 mm, and subsequent progressive BL ≥ 2–3 mm
Peri-implantitisin absence of previous examination—patient records should include previous radiographs, PD at one-year postload. In the absence of a previous exam, refer to the guidelines for peri-implantitis, PD ≥ 6 mm, BOP, and BL ≥ 3 mm with concurrent peri-implantitis diagnosis
4. Peri-implant soft- and hard-tissue deficiencies—conditions following the normal healing process of tooth loss that leads to diminished dimensions of the alveolar process/ridge, resulting in both hard- and soft-tissue deficiencies (1)
Clinical applications
The new peri-implant diseases and conditions categories are research driven and include the importance of soft-and hard-tissue deficiencies, which are relevant to the success of dental implants in the long term.
Clinical application for these guidelines starts with an assessment of the implant to diagnose its condition. Is it healthy, is mucositis present, is peri-implantitis present, or is there evidence of poor oral hygiene (OH)—i.e., is biofilm present, a lack of keratinized mucosa, (BOP), and/or suppuration?
Next, determine the proper maintenance appointment and recall visit: healthy, mucositis, or treatment for peri-implantitis. According to the American College of Prosthodontists' 2016 Clinical Practice Guidelines for Recall and Maintenance of Patients with Tooth-Borne and Implant-Borne Dental Restorations, recall needs to be provided by a dental professional at least every six months. Many other factors contribute to setting the recall appointment for implant maintenance. Is the patient a previous periodontal disease patient or a previous or current smoker? Does the patient have any other inflammatory diseases, negative habits, or any overall health concerns? (2)
Implant assessment
Assess the implant to diagnose its condition or health, including any hard- and soft-tissue deficiencies. Follow the Wingrove five-step implant assessment, which starts by assessing the tissue surrounding the implant, known as the perimucosal seal, for any inflammation that may be present. (3)
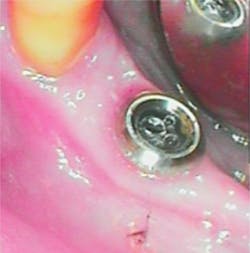
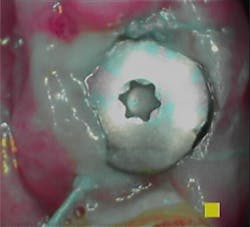
Note in the patient’s record whether any inflammation is visually present by using an intraoral camera if possible. Use the Gingival Index rating to assess the inflammation level on a scale of 1–3: mild, moderate, or severe (figures 1a–1c).
Figure 1a: PERIO Mode: Mild = Pink (Image courtesy of Acteon)
Figure 1b: PERIO Mode: Moderate = Purple Pink (Image courtesy of Acteon)
Figure 1c: PERIO Mode: Severe = Magenta Red (Image courtesy of Acteon)
Continue assessment with the use a metal or plastic probe to note any bleeding points present, and search the palate for signs of infection.
Assess for residue using dental tape or woven floss to determine if there is a need to debride—i.e., remove any calculus or residue with a titanium instrument.
Assess for mobility, pain, and/or occlusion as well as assess the bone level of the implant. Implants are held in with bone, and radiographs are needed to determine the health of the implants.A radiograph—vertical bitewing, periapical, panoramic, or 3-D cone beam—can accurately measure the crestal bone level around implant.
Once this assessment is complete, note in the patient’s record which category, according to the 2017 World Workshop Classification for Peri-Implant Diseases and Conditions, best fits the current condition of each implant.
After review of the literature, consensus reports, and based on maturation rate of bone at one year, my recommendation is to obtain a baseline probing depth and radiograph at one-year postload. This is after the implant has been restored and in function for one year. The implant will have some changes in crestal bone levels up to the first year. However, after that, there should be little change in bone level unless the implant or the overall health of the patient changes. These baseline readings allow the clinician to monitor the implant at future appointments (table 2).
Table 2: Clinical applications (peri-implant health, mucositis, implantitis), case definition, and diagnostic considerations
CLICK ON TABLE TO VIEW LARGER
Peri-implant soft- and hard-tissue deficiencies
Clinical applications related to conditions of soft- and hard-tissue deficiencies include many factors, from the patient's medical and dental history to risk factors that can affect the health of the implant. Note all the following conditions in the patient’s record.
Soft-tissue deficiency conditions that cause recession of the peri-implant mucosa: malposition of implants, thin tissue biotype, lack of keratinized tissue or buccal bone, status of periodontal attachment on adjacent teeth, and surgical tissue trauma (4)
Hard-tissue deficiency conditions: injury; longitudinal root facture; medications; previous smoker; pneumatization of the maxillary sinus; and systemic diseases reducing the amount of naturally formed bone, including periodontal disease (4)
Previous dental history factors: agenesis of teeth, loss of periodontal support, endodontic infections, thin buccal bone plate, buccal/lingual tooth position in relation to the arch, pressure from soft-tissue-supported removable prosthesis, extraction with trauma to the tissues, or a combination of factors. Monitor accordingly. (4,7)
For all patients with implant-borne restorations, include the following in their patient records: a radiograph at the time of implant placement, loading and one-year postload baseline readings. Also include a probing-depth reading in as many of the six sites as possible at one-year postload.
For all patients:Monitor your patients with a one-year postload radiograph and probing-depth readings for the life of the implant. Encourage patients to achieve keratinized tissue with stimulation using a rubber tip stimulator once daily for comfort, esthetics, and ease of plaque control. Combine this with good home care for long-term implant health benefits. (3)
References
1. Caton G, Armitage G, Berglundh T, et al. A new classification scheme for periodontal and peri‐implant diseases and conditions – Introduction and key changes from the 1999 classification. J Clin Periodontol. 2018;45(suppl 20):S1-S8. doi:10.1111/jcpe.12935.
2. Bidra AS, Daubert DM, Garcia LT, et al. Clinical practice guidelines for recall and maintenance of patients with tooth-borne and implant-borne dental restorations. J Prosthodont. 2016;25(suppl 1):S32-S40. doi:10.1111/jopr.12416.
3. Wingrove SS. Peri-Implant Therapy for the Dental Hygienist: Clinical Guide to Maintenance and Disease Complications. Oxford: UK: Wiley-Blackwell; 2013.
4. Berglundh T, Armitage G, Araujo MG, et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol. 2018;45(suppl 20):S286-S291. doi:10.1111/jcpe.12957.
5. Froum SJ, Rosen PS. A proposed classification for peri-implantitis. Int J Periodontics Restorative Dent. 2012;32(5):533-540.
6. Renvert S, Persson GR, Pirih FQ, Camargo PM. Peri‐implant health, peri‐implant mucositis, and peri‐implantitis: Case definitions and diagnostic considerations. J Clin Periodontol. 2018;45(suppl 20):S278–S285. doi:10.1111/jcpe.12956.
7. Hämmerle CHF, Tarnow D. The etiology of hard- and soft-tissue deficiencies at dental implants: A narrative review. J Periodontol. 2018;89(suppl 1):S291–S303. doi:10.1002/JPER.16-0810.