Lies, damned lies, and statistics: The truth behind the importance of flossing
Mark Twain popularized the quote: “There are three kinds of lies: lies, damned lies, and statistics.” He used this phrase to talk about the persuasive power numbers have and how they can be manipulated by individuals to push a public agenda. Mark Twain, a clairvoyant by many accounts, probably would have used this phrase to describe the recent story that has made big news regarding flossing these past few days.
Last week the Associated Press (1) released an investigative report citing “weak evidence” behind the importance of flossing. This report incited a maelstrom of articles, blogs, and interviews that have all called into question the once-obvious recommendation by dentists to their patients on the need for flossing to be included into oral hygiene routines. In fact, to date, this report has been mentioned on more than 150 different news sites, and that number continues to grow. Hundreds of patients have been asking their dentist or other dental professionals why they have been encouraged to floss if it doesn’t work.
The intent of this article is to give the history behind this investigative report, examine what the term “weak evidence” means in the larger scheme of things, and offer dental professionals talking points when your patients ask about the importance of flossing.
ADDITIONAL READING |Dental profession reacts to Associated Press report about flossing evidence
The background behind this investigative report started in 2012 when an orthodontist who was treating the son of Associated Press Reporter Jeff Donn asked if Donn would be interested in a story about flossing stating that there was no evidence that flossing worked. Donn began reviewing the research on flossing and also asked the Department of Human Health and Agricultural Services about research supporting its Dietary Guidelines for Americans on the recommendation to floss. After prodding the United States Department of Health and Human Services (HHS), Donn got a letter of response stating that the committee had done no research on flossing and that they pushed it more because of “general public health recommendation.” Shortly after the HHS issued that statement, the guidelines were changed and new ones established that did not include the recommendation to floss. This removal from the guidelines spurred Donn to write his investigative report.
In his report he goes on to state that he looked at 25 studies on flossing and most of them contained either a “weak amount of evidence” to show flossing worked, “were unreliable” in their testing methods, and/or “contained a large bias” as they were funded by flossing manufacturers. In addition, Donn goes on to say that flossing manufacturers have to pay the American Dental Association $14,500 to evaluate their products in order to receive the ADA seal of approval. Once approved there is an additional annual fee of $3,500 to continue to carry the seal. In his article he implies that there is a financial motive to keep flossing relevant.
MORE ARTICLES FROM DR. SCOTT FROUM . . .
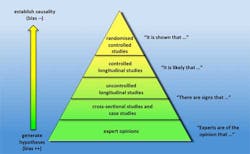
Although Donn is correct in stating that there is a paucity of good studies on flossing and many of the studies do show “a weak amount of evidence” that flossing reduces plaque and cavities, (2) he has done a big disservice to the public by not explaining what statistics mean and how they can be used to show something as obvious as the benefits of flossing are not true. When examining evidence-based medicine, typically there is a hierarchy of how studies rank in levels of credibility. The studies with the highest credibility/level of evidence are randomized controlled trials, and those with the least credibility are expert opinions (figure 1).
Figure 1: Credibility levels for evidence-based studies in medicine
In addition, these studies determine levels of evidence and credibility, with Level 1 being the most credible and Level 5 being the least credible (figure 2), since the evidence was probably derived from expert opinion or animal studies. (3) One of the problems of evidence-based medicine is the emphasis that is put on “high quality” or Level 1 evidence. Long-term, randomized controlled trials that have enough participants to mean something (sufficient power to recognize statistical/clinical significance) are very hard to conduct and can be extremely costly. Furthermore, short-term, case-controlled studies or observations of proof by professionals that are lower down in the hierarchy of credible evidence can be assigned a low level of proof or “weak evidence” simply because they are not randomized controlled trials.
Figure 2: Levels of evidence and credibility
To prove the point on how statistics can belie important data, a study was conducted on the use of parachutes to prevent bodily damage when descending from places of high altitude (i.e., jumping out of a plane). The study showed that because no randomized long-term clinical trials have been conducted on this subject, there was “a weak amount of evidence” to prove that parachutes prevented death and bodily trauma from gravitational challenges. (4) This ridiculous conclusion was based on the fact that no good studies have been conducted on this particular subject. This same ridiculous conclusion can apply to the case for floss. Of the 25 studies that Donn looked at on flossing, many were flawed. Many of these studies were either short term, not well run, participants weren’t given instructions on flossing, data was inconsistently recorded, etc. (5)
As periodontist and past president of the Florida Association of Periodontists James Wilson, DMD, explains:
When the US government removed flossing from its 2015–2020 Dietary Guidelines, it did so because the strength of the studies regarding the effectiveness of flossing was admittedly weak. They were generally short term with a small number of study participants due to the cost of running high-quality scientific studies. It makes sense that companies that sell dental floss and dental school universities are not going to pay hundreds of thousands, if not millions, of dollars for large-scale studies lasting many years to prove what most dentists and patients took as truth. Because long-term studies are so expensive, dentists have, for years, extrapolated from shorter-term ones that the buildup of plaque and increased level of inflammation that occurs when patients do not floss can, in a susceptible individual, lead to an increased amount of cavities and gum disease. These extrapolations are reinforced by what we see in our patients daily. Unfortunately, what many take from the article (written by Mr. Donn) Wednesday, is that a “lack of evidence” is somehow proof that flossing has no benefit. As in, no flossing is better than flossing if the evidence is not high quality. The bottom line is that a lack of high-quality evidence is not proof of ineffectiveness, especially when there has been little effort to obtain “high-quality” evidence.
So what is the take-home message to tell your patients when they ask if they should floss? The answer is of course you should. Let your patients know that many of the studies used to come up with the assessment by the Associated Press were flawed, short term, or not deemed credible levels of evidence for the above stated reasons. Let them know that “the evidence that flossing is beneficial is weak . . . but the evidence that it is not beneficial or harmful is even weaker.” If your patient has open contacts, multiple splinted fixed restorations, and/or doesn’t know how to use floss properly, other interdental cleaners such as water irrigators will probably be more effective than floss. While flossing may not be a big deal for some people, it likely helps many people who suffer from periodontal disease, high interproximal caries rates, and/or have expensive dental restorations such as dental implants. (6) In light of the low cost of flossing and its potential benefits, continue to recommend that patients include daily flossing or adjunctive interproximal cleaners as one part of their daily oral hygiene routine along with brushing their teeth twice a day.
When Associated Press Reporter Jeff Donn was asked during an interview if he would still floss in light of all the evidence he presented in his investigative article on flossing, his answer was yes. Interesting.
References
1. Donn J. Medical benefits of dental floss unproven. Associated Press News website. http://bigstory.ap.org/article/f7e66079d9ba4b4985d7af350619a9e3/medical-benefits-dental-floss-unproven. Published August 2, 2016. Accessed August 7, 2016.
2. Poklepovic T, Worthington HV, Johnson TM, et al.Interdental brushing for the prevention and control of periodontal diseases and dental caries in adults. Cochrane Database Syst Rev. 201318;(12): CD009857. doi: 10.1002/14651858.CD009857.pub2.
3. Burns PB, Rohrich RJ, Chung KC. The levels of evidence and their role in evidence-based medicine. Plastic Reconstr Surg. 2011;128(1):305–310. doi: 10.1097/PRS.0b013e318219c171.
4. Smith GCS, Pell JP. Parachute use to prevent death and major trauma related to gravitational challenge: systematic review of randomised controlled trials. BMJ. 2003;327(7429):1459–1461.
5. Sambunjak D, Nickerson JW, Poklepovic T, et al. Flossing for the management of periodontal diseases and dental caries in adults. Cochrane Database Syst Rev. 2011;(12):CD008829. doi: 10.1002/14651858.CD008829.pub2.
6. Jepsen S, Berglundh T, Genco R, et al. Primary prevention of peri-implantitis: managing peri-implant mucositis. J Clin Periodontol. 2015;42(Suppl)16:S152–7. doi: 10.1111/jcpe.12369.
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.