Laser therapy for bad breath: Clinical evidence and applications
What you’ll learn in this article
- The microbiological causes of oral halitosis and why tongue coating plays a central role.
- Why traditional mechanical cleaning often fails to provide lasting relief from bad breath.
- How laser therapy, including Solea CO₂ laser applications, offers a minimally invasive, long-term solution by targeting bacterial biofilm.
- Practical considerations for integrating laser halitosis treatments into your clinical workflow, including team roles and patient selection.
Bad breath affects approximately 25%–65% of the United States population, creating significant social and psychological impacts for patients.1 While traditional treatments for halitosis originating from the mouth focus on mechanical cleaning and antimicrobial rinses, emerging laser technologies offer promising alternatives for health-care professionals seeking more effective halitosis management strategies.
Recent clinical research demonstrates that both laser therapy and antimicrobial photodynamic therapy (aPDT) can effectively eliminate the microorganisms responsible for volatile sulfur compound (VSC) production, addressing the root cause of oral malodor with superior long-term results compared to conventional approaches.2 Halitosis originating from the oral region is largely thought to be the main contributor to bad breath.3 Other sources include both the digestive system and nasopharyngeal areas. This article will focus on bad breath originating from the mouth.
Understanding the microbiology of oral halitosis
Oral halitosis largely results from VSCs produced through metabolic processes of anaerobic bacteria located on the posterior dorsal tongue surface.4 These microorganisms break down proteins and amino acids, generating hydrogen sulfide, methyl mercaptan, and dimethyl sulfide—the primary contributors to oral malodor.
Traditional mechanical cleaning with tongue scrapers removes bacterial debris but fails to significantly reduce microbial populations, especially those that burrow into mucosal tissue and are hard to eradicate. This limitation explains why conventional treatments often provide only temporary relief, requiring frequent reapplication to maintain clinical efficacy.5
On the other hand, clinical studies have identified specific pathogenic bacteria that respond favorably to laser intervention.6 Key anaerobic species implicated in halitosis show significant population reduction following laser treatment, with effective bacterial elimination up to one year posttreatment.7
The sustained reduction in both anaerobic and aerobic bacterial cultures following laser therapy demonstrates the comprehensive antimicrobial effects of this treatment modality, extending beyond the immediate treatment period.
Solea CO2 laser application for bad breath
Low-power 9.3-micron CO2 laser therapy (Solea Laser, Convergent Dental) represents an alternative approach to halitosis management, utilizing different mechanisms to achieve bacterial elimination. The 9,300 nm wavelength of this CO2 laser is well absorbed by water with an excellent power to ablate and coagulate biofilm structure and has a shallow depth of penetration into soft tissue. This shallow penetration depth makes it ideal for removing tongue coating and biofilm as well as proximal soft tissue while avoiding temperature-related tissue necrosis.
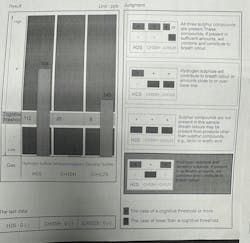
Clinical studies demonstrate sustained VSC reduction for three months following this laser treatment, significantly outperforming traditional tongue scraping methods in both immediate and long-term outcomes (figures 1 and 2).
Clinical implementation considerations
Successful integration of laser therapy for halitosis requires careful consideration of equipment selection, protocol standardization, and patient screening procedures. Health-care professionals must evaluate practice requirements and patient populations to determine optimal treatment approaches.
Implementation of laser therapy protocols requires appropriate equipment acquisition and clinical training. Solea laser tongue treatments require specific operational knowledge and instrumentation to ensure safe and effective treatment delivery without harm to soft-tissue structures.
Comparative treatment outcomes
Laser tongue debridement demonstrated superior efficacy compared to conventional mechanical cleaning methods. VSC reduction following laser treatment exceeds that achieved through tongue scraping, with sustained benefits extending beyond traditional treatment time frames.
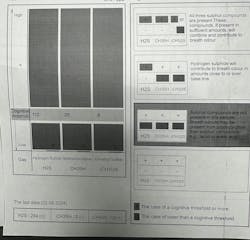
This type of low-level laser therapy modality showed immediate VSC reduction, with gas chromatography measurements confirming significant improvements in oral malodor immediately posttreatment and three months later (figures 3 and 4).
Follow-up studies extending to three months posttreatment demonstrate maintained bacterial reduction and continued VSC suppression, supporting laser therapy as a long-term halitosis management strategy.8
Conclusions
Laser therapy represents a significant advancement in halitosis management, offering health-care professionals effective tools to address this underestimated but socially significant condition. The combination of immediate efficacy and sustained bacterial elimination provides superior clinical outcomes compared to traditional mechanical approaches.
For dental professionals and health-care teams, implementing laser therapy protocols can enhance patient care quality while addressing a condition that significantly impacts patient quality of life and social functioning. The growing body of clinical evidence supports laser therapy as a minimally invasive, effective treatment modality worthy of consideration in comprehensive halitosis management strategies.
Extended follow-up studies are needed to establish the long-term sustainability of laser therapy benefits. Current research provides evidence for up to three months posttreatment, but longer observation periods would support treatment interval optimization.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
References
- Tungare S, Zafar N, Paranjpe AG. Halitosis. In: StatPearls [Internet]. StatPearls Publishing; 2025. https://www.ncbi.nlm.nih.gov/books/NBK534859/
- Woźniak A, Matys J, Grzech-Leśniak K. Effectiveness of lasers and aPDT in elimination of intraoral halitosis: a systematic review based on clinical trials. Lasers Med Sci. 2022;37(9):3403-3411. doi:10.1007/s10103-022-03656-3
- Veeresha KL, Bansal M, Bansal V. Halitosis: a frequently ignored social condition. J Int Soc Prev Community Dent. 2011;1(1):9-13. doi:10.4103/2231-0762.86374
- Shenoy N, Shetty A. Breath malodor – a review of the fundamentals. Journal of Datta Meghe Institute of Medical Sciences University. 2023;18(4):882-888. doi:10.4103/jdmimsu.jdmimsu_505_23
- Krespi YP, Kizhner V, Wilson KA, et al. Laser tongue debridement for oral malodor–a novel approach to halitosis. Am J Otolaryngol. 2021;42(1):102458. doi:10.1016/j.amjoto.2020.102458
- Poormoradi B, Gholami L, Fekrazad R, et al. Comparison of the effect of Er,Cr:YSGG laser and Halita mouthwash on oral malodor in patients with chronic periodontitis: a randomized clinical trial. J Lasers Med Sci. 2021;12:e26. doi:10.34172/jlms.2021.26
- Waikar VR, Pankey N, Lohe V. Laser therapy: an alternative approach for the management of halitosis. Cureus. 2024;16(7):e65911. doi:10.7759/cureus.65911
- Froum SH, et al. 9.3 Micron CO2 laser tongue debridement to control oral halitosis. A case series. Manuscript in preparation.
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.