Insulin resistance and dental health: Why dentists are the first line of defense
Key Highlights
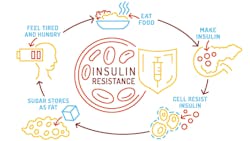
- Early detection in the dental chair: Dentists and hygienists can spot oral signs of insulin resistance—such as chronic gingival inflammation, delayed healing, or unexplained tooth mobility—often years before diabetes develops.
- Two-way link between gums and glucose: Periodontal disease and insulin resistance fuel each other through systemic inflammation, diet changes, and microbial imbalances that worsen both oral and metabolic health.
- Prevention through collaboration: Dental professionals play a vital role in screening, educating, and referring patients for metabolic evaluation—helping reverse insulin resistance through early intervention, nutrition, and lifestyle support.
Dentists and allied dental health professionals can often be the first health-care providers to detect signs of systemic inflammation—bleeding gums, delayed healing, recurrent abscesses, or unexplained tooth mobility. By recognizing that these findings might also reflect insulin resistance, a patient’s long-term health trajectory can be changed. Insulin resistance (IR) may silently predate diabetes by 10 to 15 years, giving dental professionals a unique window of opportunity to intervene early.1
How is insulin resistance measured?2
Insulin resistance is measured indirectly through tests like the HOMA-IR (Homeostatic Model Assessment) or by evaluating blood sugar levels and other risk factors. Numbers indicating insulin resistance include a fasting blood glucose level of 1 or higher, an A1C between 5.7% and 6.4%, an LP-IR score optimally less than 50, or a HOMA-IR score greater than 1.75.
What are the risk factors for insulin resistance?
Insulin resistance can’t be identified by appearance alone. While overweight and obese individuals may be at increased risk, many normal-weight individuals also exhibit IR.
Key risk factors include3:
- Blood pressure readings of 130/80 or higher
- A fasting glucose level over 100 milligrams per deciliter (mg/dL)
- Elevated HbA1c above 5.7%
- A fasting triglyceride level over 150 mg/dL
- An HDL cholesterol level under 40 mg/dL in men and 50 mg/dL in women
- Skin tags
- Patches of dark, velvety skin under the arms or on the neck (acanthosis nigricans)
- Damage to tiny blood vessels in the backs of the eyes, which can lead to a condition called retinopathy
- Chronic gingival inflammation, rapid bone loss, and delayed healing without local etiology (bacteria)
Insulin resistance’s influence on periodontal disease and tooth loss
A study examining more than 8,000 participants found that people with the most missing teeth were 30% more likely to exhibit insulin resistance.4 Poor diet quality and elevated systemic inflammatory markers partly mediated this link. For example, tooth loss, often resulting from periodontal disease, reduces masticatory function, promotes soft-food diets low in fiber and antioxidants, and fuels systemic inflammation. The outcome is a self-perpetuating cycle: fewer teeth → poorer diet → higher inflammation → worsening insulin resistance.
Another study demonstrated how oral pathogens such as Porphyromonas gingivalis and Tannerella forsythia directly impair insulin signaling through endotoxin-driven inflammation, oxidative stress, adipokine imbalances, and microbial translocations leading to infection and inflammation.5 Together, these mechanisms explain how chronic periodontitis can act not only as a symptom but also as a driver of insulin resistance.
Further reading: Type 5 diabetes (severe insulin-deficient diabetes): What every dental professional should know
How can patients reverse insulin resistance?
Insulin resistance is reversible. Early lifestyle modifications can restore cellular insulin sensitivity and benefit both oral and systemic health:
- Exercise regularly: Physical activity is one of the strongest insulin sensitizers. Skeletal muscle plays a primary role in managing the body's glucose levels by acting as the main site for glucose uptake from the bloodstream. This process is crucial for maintaining blood glucose homeostasis. The regulation of glucose uptake in muscle is a complex, three-step process that is primarily controlled by insulin and physical activity.6.7
- Achieve healthy weight: Modest weight loss reduces pancreatic strain and improves glucose uptake.
- Eat for metabolic balance: Favor nonstarchy vegetables, whole grains, fruits, and lean proteins. Limit processed sugars and saturated fats. Eat polyphenols—found in green tea, berries, cocoa, grapes, and herbs—to combat both periodontal inflammation and insulin resistance. Their antioxidant and antimicrobial properties reduce gingivalis colonization, improve endothelial health, and restore insulin sensitivity.
- Sleep and stress management: Adequate sleep and stress reduction blunt cortisol spikes that worsen insulin resistance.
Why should dental care providers screen for insulin resistance?
- Early detection saves years: Insulin resistance precedes type 2 diabetes by up to 15 years; identifying it early can prevent micro- and macrovascular damage.
- Shared inflammatory pathways: Treating periodontal inflammation helps lower systemic cytokine load, potentially improving insulin sensitivity.
- Patient education: Discussing metabolic risk during dental visits reinforces the concept of the mouth-body connection and motivates lifestyle change.
- Interdisciplinary collaboration: Timely referral to primary-care physicians or endocrinologists enables early lab testing (fasting glucose, HOMA-IR, LP-IR score lipid panel).
Conclusion
Insulin resistance isn’t just an endocrinologist’s problem—it’s a dental concern. For the practicing dentist, recognizing signs of IR offers a unique opportunity to prevent diabetes, reduce inflammation, and preserve both teeth and systemic health. By identifying risk early, coordinating with physicians, and guiding patients toward anti-inflammatory, polyphenol-rich nutrition and healthy habits, dentists can treat beyond the tooth—protecting health, not just smiles.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
References
- Tabák A, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379(9833):2279-2290. doi:10.1016/S0140-6736(12)60283-9
- Insulin resistance and prediabetes. Blood tests. National Institutes of Health. National Institute of Diabetes and Digestive and Kidney Diseases. Reviewed March 2025. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance
- Booth S. Insulin resistance — what you need to know. WebMD. Reviewed April 22, 2024. https://www.webmd.com/diabetes/insulin-resistance-syndrome
- Hao Y, Li S, Dong S, Niu L. The association between tooth loss and insulin resistance mediated by diet quality and systemic immunoinflammatory index. Nutrients. 2023;15(23):5008. doi:10.3390/nu15235008
- Thouvenot K, Turpin T, Taïlé J, Clément K, Meilhac O, Gonthier MP. Links between insulin resistance and periodontal bacteria: insights on molecular players and therapeutic potential of polyphenols. Biomolecules. 2022;12(3):378. doi:10.3390/biom12030378
- Motamed B, Kohansal Vajargah M, Kalantari S, Shafaghi A. HOMA-IR index in nondiabetic patient, a reliable method for early diagnosis of liver steatosis. Caspian J Intern Med. 2022;13(3):519-526. doi:10.22088/cjim.13.3.519
- Merz KE, Thurmond DC. Role of skeletal muscle in insulin resistance and glucose uptake. Compr Physiol. 2020;10(3):785-809. doi:10.1002/cphy.c190029
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.

Benjamin S. González, MD
Benjamin S. González, MD, an integrative and functional medicine physician, is a graduate of the University of Arizona College of Medicine. He served in both the Air Force and the Army with multiple overseas deployments. Dr. González is founder and medical director of Atlantis Medical Wellness Center in Silver Spring, Maryland. His background in genetics, nutrition, obesity medicine, hormone replacement, and metabolic medicine gives him a powerful perspective for wellness care. Contact him @bengonzalez_md.