A technique to improve the viral protection of a procedure mask in absence of an N95 shield respirator
by Chandur P.K. Wadhwani, BDS, MSD
Paul S. Rosen, DMD, MS
Ari S. Rosen
Yasmin H. Wadhwani
Kwok-Hung Chung, DDS, PhD
Abstract
The coronavirus disease 2019 (COVID-19) outbreak is a pandemic problem that is stretching the limits of medical and dental professionals to effectively and safely deliver health care. Personal protective equipment (PPE) is in short supply. As the contagion of this virus is spread through aerosol droplets, respiratory protection for health-care providers is an integral part of infection control. Since there is a shortage of masks, we offer our colleagues a novel technique to improve upon respiratory protection under the current circumstances.
Introduction
Face masks are an indispensable technology when dealing with a pandemic, especially as they offer protection against respiratory infections.1 While a surgical mask may be effective in blocking splashes and large-particle droplets, by design a face mask does not filter or block very small particles in the air that may be transmitted by coughs, sneezes, or certain medical procedures. Surgical masks also do not provide complete protection from germs and other contaminants due to the loose fit between the surface of the face mask and the face.2 Surgical face masks are not designed for protection from viral carriers, such as influenza and other viruses as well as the more recently discovered COVID-19—viruses which are believed to spread by aerosol transmission.3-5
The current COVID-19 outbreak is one such example of a virus that can become lethal, spreading through aerosolized droplets and infecting anyone in close proximity. In medicine, and most certainly dentistry, we must treat patients with procedures that create aerosolization of these potentially lethal pathogens.3-5 To combat this problem, the Centers for Disease Control and Prevention (CDC)5 has suggested that N95 masks be worn along with a surgical gown, drape, and surgical gloves, as well as other protective measures.6-8
An N95 respirator is a protective device designed for efficient filtration of airborne particles by providing a very close facial fit. These devices should ideally form a seal around both the nose and mouth. The N95 version designed for medical use is meant to protect both patients and health-care personnel from the transfer of microorganisms, body fluids, and particulate material. Surgical N95 respirators are class II devices regulated by the Food and Drug Administration under 21 CFR 878.4040, and CDC NIOSH under 42 CFR Part 84.2
Many clinicians, when faced with treating emergency patients in a climate in which these masks are in short supply,9,10 have been left to decide whether to wear suboptimal protection such as traditional procedure masks, to provide care that may not solve the problem by avoiding steps within the procedure that may create aerosolization, to seek out someone else who may have the proper equipment, or—as last resorts—to create a makeshift mask with available materials or send the patient to the emergency room. It has recently been reported that the CDC has also relaxed its specifications related to the N95 mask, such as its ability to fit and seal to the face.11
Technique
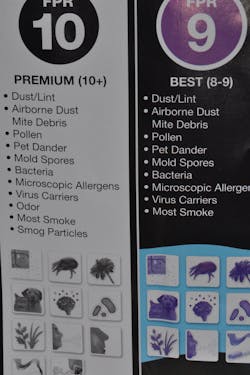
This technique can be used to enhance a level 3 or exam mask to provide increased protection.
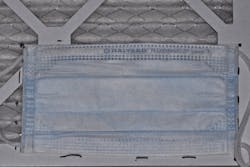
2. Outline the size of the mask onto the air filter (figure 2).
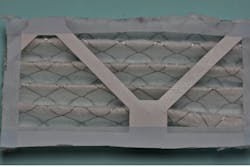
3. Remove the surgical mask, place surgical/hypoallergenic tape over the markings, and cut the air filter to shape. The filter will be placed on the outside of the mask, so it should be cut to the dimensions of the mask (figure 3a). Note that the wire mesh may be sharp; tape should be used to help prevent injury. Cut through the cardboard support material as this restricts the concertina effect of the filter (figure 3b).
7. To add further protection and prevent the mask from moving, secure the edges with more surgical tape to improve the seal (figures 7a and 7b).
Discussion
Another level of scrutiny concerns qualitative and quantitative fit testing of half masks, such as those that only cover the nose and mouth. Qualitative tests include those that detect leakage of isoamyl acetate (which smells like bananas), saccharin (which leaves a sweet taste in one’s mouth), Bitrex (which leaves a bitter taste), and irritant smoke (which can cause coughing).
The advantage of this face mask modification technique is that it will still allow health-care professionals to continue to wear their standard eye protection, whether that be eyeglasses, loupes, or a face shield. Masks have historically been important as a physical barrier against aerosolization, which occurs in a number of medical and dental procedures.5,6,8,11 While more of this emphasis has been on the physical and visual aspects along with bacteria, as we move forward we are realizing that we must be cognizant of their implication with viruses.3,4
It is suggested that filters in heating and air-conditioning systems be changed every 90 days. The authors are not advocating this as the use of this filter is different and not validated for this length of time. It should be noted that, in theory, viruses can be transmitted through means other than aerosol, such as large droplets or direct contact with secretions (or fomites). The need for good hand hygiene as reported by the World Health Organization and the FDA, in addition to routine use of adequate PPE, cannot be overemphasized.7,8
Summary
Authors’ note: The authors are providing this information in light of the severe shortage of N95 masks. In no way are the authors stating that this technique has been validated, nor are they advocating the use of this mask instead of an N95 mask if it is available. Each individual must decide what to do given the risks and benefits to themselves and their patients.
Read more about COVID-19: COVID-19: Flattening the curve—the best offense is a good defense
References
1. MacIntyre CR, Chughtai AA. Facemasks for the prevention of infection in healthcare and community settings. BMJ. 2015;350:h694. doi:10.1136/bmj.h694
2. Respiratory protection. Occupational Safety and Health Administration. https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.134
3. Tellier R. Review of aerosol transmission of influenza A virus. Emerg Infect Dis. 2006;12(11):1657-1662.
4. Judson SD, Munster VJ. Nosocomial transmission of emerging viruses via aerosol-generating medical procedures. Viruses. 2019;11(10):940. doi:10.3390/v11100940
5. Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135(4):429-437. doi:10.14219/jada.archive.2004.0207
6. WHO guidelines on hand hygiene in health care. World Health Organization. 2009. Accessed March 22, 2020. http://www.who.int/gpsc/5may/tools/9789241597906/en/index.html
7. N956 respirators and surgical masks (face masks). US Food and Drug Administration. Updated March 11, 2020. https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-respirators-and-surgical-masks-face-masks
8. Smith JD, MacDougall CC, Johnstone J, Copes RA, Schwartz B, Garber GE. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis. CMAJ. 2016;188(8):567-574. doi:10.1503/cmaj.150835
9. Face mask shortage prompts CDC to loosen coronavirus guidance. The Washington Post. March 10, 2020. Accessed March 22, 2020. https://www.washingtonpost.com/health/2020/03/10/face-mask-shortage-prompts-cdc-loosen-coronavirus-guidance
10. Goodnough A. Some hospitals are close to running out of crucial masks for coronavirus. The New York Times. March 9, 2020. https://www.nytimes.com/2020/03/09/health/coronavirus-n95-face-masks.html
11. Updated CDC guidance on use of N95 respirators by healthcare workers. Tennessee State Government. Accessed March 22, 2020. https://www.tn.gov/content/dam/tn/health/documents/N95.pdf
Editor’s note: This article originally appeared in Perio-Implant Advisory, a newsletter for dentists and hygienists that focuses on periodontal- and implant-related issues. Perio-Implant Advisory is part of the Dental Economics and DentistryIQ network. To read more articles, visit perioimplantadvisory.com, or to subscribe, visit dentistryiq.com/subscribe.