Vitamin D and COVID-19 disease severity: An old ally in a new war
SARS-CoV-2 is a coronavirus in the β-CoV family that is a single-stranded, large, enveloped RNA virus.1 Common symptoms of COVID-19 can range from mild to severe and include cough, fever, myalgia, fatigue, chest pain, loss of smell and/or taste, trouble breathing, headaches, sore throat, chills, diarrhea, nausea, and vomiting.2 Progression of this disease can result in pneumonia, with critical disease severity resulting in respiratory failure from acute respiratory distress syndrome (ARDS). This virus can also cause organ failure mediated by a hyperinflammatory cytokine storm.3 Medical conditions associated with an increase in the severity of this disease include hypertension, obesity (BMI > 30), diabetes mellitus type 2, cardiac disease, respiratory diseases, chronic kidney disease, asthma, chronic lung disease, liver disease, and individuals who are immunocompromised.
In one of the largest studies on hospitalized COVID-19–positive patients, increased age (65 and older), and those with more than one comorbidity were found to comprise 90% of the presenting patients.4 Studies have shown that 80%–85% of people who contract SARS-CoV-2 will be either asymptomatic or have mild symptoms. Another 13% will develop moderate symptoms, and 5% will develop severe symptoms.5 Recent studies have demonstrated a correlation between lower levels of vitamin D and increased disease severity.
This article will briefly examine the role vitamin D plays in viral immunity and present the evidence that proper levels of vitamin D may decrease the severity of COVID-19.
Vitamin D in its inactive form (vitamin D3 or cholecalciferol) is a steroid hormone that is synthesized in the skin with adequate exposure to the sun (UVB light), acquired through diet, and/or vitamin supplementation. Vitamin D is considered deficient when serum 25(OH) levels are less than 10 ng/mL, insufficient when serum levels are 10–30 ng/mL, and optimal with serum levels greater than 30 ng/mL. Additionally, vitamin D is a key player in bone growth and metabolism, cognitive function, cardiovascular health, as well as health of the respiratory tract, skin, and the endocrine system.
Vitamin D also plays a major role in both the innate and acquired immune system with a substantial function in bacterial and viral defense. Vitamin D reduces the risk of viral and microbial infection by three distinct mechanisms: physical barrier, innate immunity, and adaptive immunity:
- Physical barrier: Vitamin D helps maintain tight junctions, gap junctions, and adherens junctions that prevent bacterial and viral entry into the cell.6
- Innate immunity: Vitamin D enhances cellular innate immunity partly through the induction of antimicrobial and antiviral peptides such as cathelicidins and defensins. Cathelicidins target both gram-positive and gram-negative bacteria, enveloped and nonenveloped viruses, and fungi. They disturb pathogen cell membranes and target endotoxin. In addition, they reduce viral replication.7
- Adaptive immunity: Vitamin D is a modulator of adaptive immunity by suppressing the more damaging generalized pro-inflammatory Th1 cell response and shifting to a more targeted Th2 cell response, as well as facilitating T regulatory cells.8
As it relates to COVID-19, one of the more important roles vitamin D can play is in the inhibition of the cytokine storm caused by the innate immune system’s reaction to SARS-CoV-2. Vitamin D reduces the expression of pro-inflammatory Th1 cytokines, such as tumor necrosis factor–alpha, interleukin-1 (IL-1), IL-6, IL-17, and IL-21. In addition, vitamin D upregulates anti-inflammatory cytokines such as IL-10.10
In one preprint study, researchers analyzed data from 10 countries looking at C-reactive protein (CRP), a diagnostic marker of the cytokine storm. CRP was found to be inversely proportional to vitamin D levels. The study concluded that patients with deficient vitamin D levels who contracted COVID-19 were more likely to be affected by unmitigated hyperinflammation with higher mortality rates.11
In another study, researchers evaluated the serum vitamin D levels of 212 COVID-19–positive patients as they related to disease severity.12 Of the patients with normal vitamin D levels, 85% exhibited mild symptoms of the virus. Of the patients with deficient vitamin D levels, 40% experienced severe symptoms. This study concluded that the odds of having a mild clinical outcome increase when serum (OH)D levels increase. Alternatively, the odds of having a critical outcome increase when serum (OH)D levels decrease.
Vitamin D and dental considerations
The first step for dental care providers when treating patients who lack sufficient levels of vitamin D is to diagnose the serum levels as deficient, insufficient, or normal. Whole blood finger sticks are easy tests to implement in the dental office with adherence to state-mandated regulations (figures 2–4).References
- Lu R, Zhao X, Li J, et al. Genomic characterization and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565-574. doi:10.1016/S0140-6736(20)30251-8
- Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi:10.1001/jama.2020.1585
- Ye Q, Wang B, Mao J. The pathogenesis and treatment of the ‘cytokine storm’ in COVID-19. J Infect. 2020;80(6):607-613. doi:10.1016/j.jinf.2020.03.037
- Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052-2059. doi:10.1001/jama.2020.6775
- Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. Published online March 27, 2020. doi:10.1001/jamacardio.2020.1286
- Schwalfenberg GK. A review of the critical role of vitamin D in the functioning of the immune system and the clinical implications of vitamin D deficiency. Mol Nutr Food Res. 2011;55(1):96-108. doi:10.1002/mnfr.201000174
- Herr C, Shaykhiev R, Bals R. The role of cathelicidin and defensins in pulmonary inflammatory diseases. Expert Opin Biol Ther. 2007;7(9):1449-1461. doi:10.1517/14712598.7.9.1449
- Aranow C. Vitamin D and the immune system. J Investig Med. 2011;59(6):881-886. doi:10.2310/JIM.0b013e31821b8755
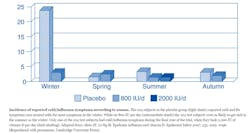
- Aloia JF, Li-Ng M. Epidemic influenza and vitamin D. Epidemiol Infect. 2007;135(7):1095-1096. doi:10.1017/S0950268807008308
- Sharifi A, Vahedi H, Nedjat S, Rafiei H, Hosseinzadeh-Attar MJ. Effect of single-dose injection of vitamin D on immune cytokines in ulcerative colitis patients: a randomized placebo-controlled trial. APMIS. 2019;127(10):681-687. doi:10.1111/apm.12982
- Daneshkhah A, Agrawal V, Eshein A, Subramanian H, Roy HK, Backman V. The possible role of vitamin D in suppressing cytokine storm and associated mortality in COVID-19 patients. medRxiv. 2020;4(8):20058578. doi:10.1101/2020.04.08.20058578
- Alipio M. Vitamin D supplementation could possibly improve clinical outcomes of patients infected with coronavirus-2019 (COVID-19). April 9, 2020. doi:10.2139/ssrn.3571484
- Grant WB, Lahore H, McDonnell SL, et al. (2020). Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020;12(4):988. doi:10.3390/nu12040988
- Wang J, Zhou JJ, Robertson GR, Lee VW. Vitamin D in vascular calcification: a double-edged sword? Nutrients. 2018;10(5):652. doi:10.3390/nu10050652
Editor’s note: This article originally appeared in Perio-Implant Advisory, a newsletter for dentists and hygienists that focuses on periodontal- and implant-related issues. Perio-Implant Advisory is part of the Dental Economics and DentistryIQ network. To read more articles, visit perioimplantadvisory.com, or to subscribe, visit dentistryiq.com/subscribe.
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.