Tooth pain after root canal therapy: The 5 common causes
Patients often expect to have immediate pain relief following endodontic therapy. Depending upon the size of the periapical lesion, necrotic state of the pulp, and the medical history of the patient, complete healing postendodontic treatment can vary. The literature reports that 3%–6% of patients can experience severe pain after root canal therapy, but this typically subsides within a week following treatment.1
Frustration can ensue, however, when pain persists (lasting longer than a week), and a common question from patients is, “I had a root canal, so why am I still in pain?” One meta-analysis reports that 5% of patients may experience pain that can last six months or longer after root canal therapy.2
To prevent patients from experiencing long-lasting pain, it is important to recognize and diagnose the potential etiology of pain following root canal treatment, especially since the origin can be multifactorial and nonodontogenic. The literature suggests that early identification and treatment of pain can lead to more effective therapeutic outcomes.3
Top 5 reasons why tooth pain may exist after root canal therapy:
No. 1: Occlusion
A high bite, malocclusion, and/or increased stress of the tooth crown from parafunction can cause inflammation of the periodontal ligament, which is not affected when the pulp is removed by a root canal. The periodontal ligament fibers remain intact and can transmit forces to the bone that mimic tooth pain. Adjusting the treated tooth may be a simple method to alleviate this problem.
No. 2: Endodontic
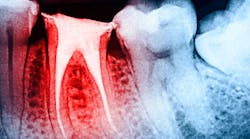
Teeth, especially multirooted teeth, can have more than one canal system. Canals that are hard to find or calcified can be missed, leading to pulp tissue that is not fully removed. In addition, teeth can have accessory canals that can be missed during root canal therapy, which can lead to posttreatment pain.4 Root and furcation perforations, irrigant irritation, filling material extrusion, and broken instrumentation in the canal system are all intraoperative problems that can lead to pain following a root canal. An examination by an endodontist may be necessary to diagnose these conditions.
No. 3: Fracture
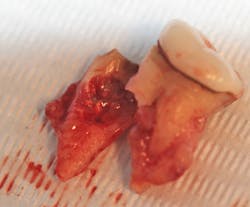
Root fracture is a common source of pain after root canal treatment and is of particular concern since it may be hard to diagnose (figure 1).5 Although new technologies such as three-dimensional imaging and microscopes have increased diagnostic ability, vertical fractures can still be hard to ascertain. Isolated periodontal pockets and a history of sharp pain that progresses to a dull throbbing pain upon mastication/palpation are common signs of fracture. Other common risk factors for fracture include: the lower second molar (most likely tooth to fracture), parafunctional habits including clenching/bruxism, large amalgam restorations, thermal injury, psychological stress, teeth with existing erosion, abrasion, and/or abfraction. A fractured tooth may need to be extracted to alleviate symptoms of pain (figure 2).
No. 4: Periodontal
The periodontium surrounding the tooth can be a source of pain, especially if there is a concurrent periodontal lesion along with an endodontic lesion (figure 3). The tooth should be clinically examined and radiographs taken following root canal treatment to evaluate both hard and soft tissue. Hard-tissue defects, such as intrabony defects and furcation involvement, can cause inflammation leading to tooth pain. In addition, soft-tissue recession can expose root surfaces, which can then lead to sensitivity and tooth pain. Food impaction, especially if the tooth is temporized, can also mimic tooth pain. Gingival irritation from the rubber dam clamp used during the root canal can simulate tooth pain, but it is usually temporary and can be alleviated with rinses or medicaments. Referral to a periodontist may be required for pain of periodontal origin.
No. 5: Nonodontogenic
Persistent pain after root canal therapy can be likely if the etiology of the pain is not tooth related. The literature suggests that 3%–5% of tooth pain can be of nonodontogenic origin.6 Temporomandibular joint dysfunction, maxillary sinusitis, neoplasms, and nonodontogenic cystic lesions can all mimic tooth pain.7 Pain syndromes stemming from shingles, trigeminal neuralgia, idiopathic periodontalgia/odontalgia, and phantom tooth pain have also been reported to be psychogenic aspects of tooth pain that could persist after root canal treatment.8 Many more nonodontogenic causes of tooth pain exist but are out of the scope of this article, and appropriate referral to a medical provider is suggested.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
References
- Sathorn C, Parashos P, Messer H. The prevalence of postoperative pain and flare‐up in single‐ and multiple‐visit endodontic treatment: a systematic review. Int Endod J. 2008;41(2):91-99. doi:10.1111/j.1365-2591.2007.01316.x
- Nixdorf DR, Moana-Filho EJ, Law AS, McGuire LA, Hodges JS, John MT. Frequency of persistent tooth pain after root canal therapy: a systematic review and meta-analysis. J Endod. 2010;36(2):224-230. doi:1016/j.joen.2009.11.007
- Vanotti A, Osio M, Mailland E, Nascimbene C, Capiluppi E, Mariani C. Overview on pathophysiology and newer approaches to treatment of peripheral neuropathies. CNS Drugs. 2007;21(Suppl 1)3-12. doi:2165/00023210-200721001-00002
- Tabassum S, Khan FR. Failure of endodontic treatment: the usual suspects. Eur J Dent. 2016;10(1):144-147. doi:4103/1305-7456.175682
- Khasnis SA, Kidiyoor KH, Patil AB, Kenganal SB. Vertical root fractures and their management. J Conserv Dent. 2014;17(2):103-110. doi:4103/0972-0707.128034
- Nixdorf DR, Moana-Filho EJ, Law AS, et al. Frequency of nonodontogenic pain after endodontic therapy: a systematic review and meta-analysis. J Endod. 2010;36(9):1494-1498. doi:1016/j.joen.2010.06.020
- Little RE, Long CM, Loehrl TA, Poetker DM. Odontogenic sinusitis: a review of the current literature. Laryngoscope Investig Otolaryngol. 2018;3(2):110-114. doi:1002/lio2.147
- Harris M. Psychogenic aspects of facial pain. Br Dent J. 1974;136(5):199-202. doi:1038/sj.bdj.4803155
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.
Omar Ikram, MRD, MClinDent, BDS, FRACDS
Omar Ikram, MRD, MClinDent, BDS, FRACDS, is an endodontist and practice owner of Specialist Endo Crows Nest based in Sydney, Australia's lower North Shore. He is also on staff at the Sydney Dental Hospital and is the president of the Australian Society of Endodontology—New South Wales Branch. Dr. Ikram completed his BDS in 1997 at Otago University and worked for approximately 10 years as a general dentist in New Zealand and England. His interest in endodontics led him to study a master's in clinical dentistry in endodontology at Kings College London, United Kingdom, followed by a Membership in Restorative Dentistry in the Royal College of Surgeons of Edinburgh. Contact him on Facebook and Instagram.