Hyperbaric oxygen therapy (HBOT) is a medical treatment that specializes in delivering pure oxygen to the body at higher-than-normal atmospheric pressures, usually in the range of 1.3 to 1.6 atmospheres (atm) for commercial-grade chambers and 2.4 atm and higher for hospital-grade chambers. Normal atmospheric air at sea level is 1 atm and 21% oxygen. Atmospheric pressure decreases as we increase elevation (climb up a mountain) and increases as we descend below sea level (submerge into the ocean).
HBOT involves breathing 100% oxygen (in a hard chamber or with a breathing apparatus in a soft chamber) while in a special space that pressurizes the air with a compressor called a hyperbaric chamber. This increase in pressure and oxygen purity has therapeutic benefits as it allows the body to absorb more oxygen than when at normal sea level. This increased oxygen saturation can help accelerate the healing process, reduce inflammation, and promote new vascular growth.1
In addition, HBOT has been found to activate fibroblast cells (cells responsible for collagen production) and encourage the development of new bone via the activation of osteoblasts. It can help reduce swelling, and, because of the increase in oxygen concentration in the blood and tissue, it can improve healing and wound care.
You may also be interested in … Red light therapy: A comprehensive overview for dental professionals
How is the hyperbaric chamber used?
Chambers can be divided into soft-shell chambers and hard-shell chambers. Soft-shell hyperbaric chambers are portable, inflatable bags made of plastic fibers such as polyurethane with steel frames (figure 1). Soft shells typically have a limit of around 1.3 atm and 30% oxygen delivery, but they can deliver 100% oxygen with a supplemental breathing apparatus.
OxyHealth is seeking FDA clearance for newer, more secured soft chambers at 1.6 atm to 1.9 atm (figure 2). They are significantly less expensive than hard chambers. Hard-shell chambers are made of steel and typically reach 1.5 atm to 3.0 atm, although some can reach 6 atm (figure 3). Most hospital settings use hard-shell hyperbaric oxygen chambers.
Medical uses for HBOT
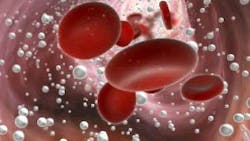
The main purpose of HBOT is to increase the amount of oxygen that reaches damaged tissue, and this happens in two primary ways. First, HBOT ionizes the oxygen molecule, allowing it to travel in the bloodstream unbound to hemoglobin, reaching damaged tissues that are typically inaccessible to larger red blood cells (figures 4 and 5).2
Second, the increased atmospheric pressure causes hemoglobin, a protein found in red blood cells, to release more oxygen than normal. This additional oxygen helps speed up healing and fight infections.
HBOT has been used to treat cognitive impairment due to traumatic brain injury, stroke, Alzheimer’s disease, and Parkinson’s disease.3 Because of increases in oxygen delivery and angiogenic response, HBOT has been used to treat chronic diabetic wounds and ulcers,4 improve skin grafting in burn victims, and promote adaptation of skin grafts and limb transplants.5 HBOT has also been studied in an antiaging capacity and has demonstrated the ability to increase telomere length by 20%, increase the percentage of circulating stem cells, and affect the antiaging pathways of SIRT 1, MTOR, and AMPK.6
One study has shown that 20 sessions of two-hour treatments at 2 atm increase circulating stem cells eightfold, or 800%.7 The antibacterial properties of HBOT make this treatment a useful adjunct in treating refractory osteomyelitis and osteoradionecrosis, as well as preventing sepsis during wound care.8
Dental uses for HBOT
Since HBOT stimulates angiogenesis, collagen synthesis, soft-tissue wound healing, and is antibacterial, it has been proposed to help with medically related osteonecrosis of the jaw.9 In addition, because of HBOT’s antibacterial properties against anaerobic bacteria, it has been successfully used to treat aggressive periodontal disease.10
Another study evaluating 20 test patients receiving HBOT for one hour at 1.4 atm for 20 sessions compared to those who did not receive HBOT found an overall improvement in both oral health indexes (e.g., plaque scores, gingival bleeding, probing depth, mobility) as well as general health.11 Preliminary animal studies show HBOT to have a positive effect on osseointegration in medically compromised animals.12
One case study looked at 10 sessions of HBOT for one hour at 2.2 atm (three sessions before implant therapy and seven sessions after implant therapy) in a patient with severe periodontal disease who received immediate zirconia implants. All implants were integrated and deemed successful one year after implant therapy.13
Other human studies have shown no benefit on dental implant failure rates when treating patients who received head and neck radiation for cancer with HBOT.14 There is a lack of studies in dentistry analyzing HBOT’s effects on dental implant therapy.15
More dental studies are needed
As with any treatment, HBOT should be discussed thoroughly with the patient prior to beginning therapy. Careful monitoring of oxygen saturation levels is also recommended during treatment. Overall, HBOT may provide a helpful adjunct for many dental conditions and can help improve overall patient outcomes. However, many more studies are needed in the dental field to ascertain the true benefit of treating dental patients with HBOT.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
References
- Thom S, et al. Hyperbaric oxygen therapy: a review of the evidence and clinical implications. Br J Hosp Med. 2016;77(7):454-458.
- Francis A, Baynosa RC. Hyperbaric oxygen therapy for the compromised graft or flap. Adv Wound Care (New Rochelle). 2017;6(1):23-32. doi:10.1089/wound.2016.0707
- Bonafide C, et al. The use of hyperbaric oxygen therapy for stroke recovery: a systematic review and meta-analysis. Neurorehabil Neural Repair. 2020;34(7):551-563.
- Miller M, et al. Hyperbaric oxygen therapy for the management of chronic non-healing wounds: a systematic review and meta-analysis. Wound Repair Regen. 2019;27(3):514-527.
- Vinkel J, Holm NFR, Jakobsen JC, Hyldegaard O. Effects of adding adjunctive hyperbaric oxygen therapy to standard wound care for diabetic foot ulcers: a protocol for a systematic review with meta-analysis and trial sequential analysis. BMJ Open. 2020;10(6):e031708. doi:10.1136/bmjopen-2019-031708
- Hachmo Y, Hadanny A, Abu Hamed R, et al. Hyperbaric oxygen therapy increases telomere length and decreases immunosenescence in isolated blood cells: a prospective trial. Aging (Albany NY). 2020;12(22):22445-22456. doi:10.18632/aging.202188
- Thom SR, Bhopale VM, Velazquez OC, Goldstein LJ, Thom LH, Buerk DG. Stem cell mobilization by hyperbaric oxygen. Am J Physiol Heart Circ Physiol. 2006;290(4):H1378-H1386. doi:10.1152/ajpheart.00888.2005
- Goerger E, Honnorat E, Savini H, et al. Anti-infective therapy without antimicrobials: apparent successful treatment of multidrug resistant osteomyelitis with hyperbaric oxygen therapy. IDCases. 2016;6:60-64. doi:10.1016/j.idcr.2016.09.008
- Freiberger JJ. Utility of hyperbaric oxygen in treatment of bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg. 2009;67(5 Suppl):96-106. doi:10.1016/j.joms.2008.12.003
- Chen TL, Xu B, Liu JC, et al. Effects of hyperbaric oxygen on aggressive periodontitis and subgingival anaerobes in Chinese patients. J Indian Soc Periodontol. 2012;16(4):492-497. doi:10.4103/0972-124X.106880
- Burcea A, Mihai LL, Bechir A, Suciu M, Bechir ES. Clinical assessment of the hyperbaric oxygen therapy efficacy in mild to moderate periodontal affections: a simple randomised trial. Medicina (Kaunas). 2022;58(2):234. doi:10.3390/medicina58020234
- Altug HA, Tatli U, Coskun AT, et al. Effects of hyperbaric oxygen treatment on implant osseointegration in experimental diabetes mellitus. J Appl Oral Sci. 2019;26:e20180083. doi:10.1590/1678-7757-2018-0083
- Giacon TA, Giancola F, Paganini M, Tiengo C, Camporesi EM, Bosco G. Hyperbaric oxygen therapy and A-PRF pre-treated implants in severe periodontitis: a case report. Int J Environ Res Public Health. 2021;18(2):413. doi:10.3390/ijerph18020413
- Condezo AFB, Araujo RZ, Koga DH, Curi MM, Cardoso CL. Hyperbaric oxygen therapy for the placement of dental implants in irradiated patients: systematic review and meta-analysis. Br J Oral Maxillofac Surg. 2021;59(6):625-632. doi:10.1016/j.bjoms.2020.08.050
- Esposito M, Worthington HV. Interventions for replacing missing teeth: hyperbaric oxygen therapy for irradiated patients who require dental implants. Cochrane Database Syst Rev. 2013;2013(9):CD003603. doi:10.1002/14651858.CD003603.pub3
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.