Magnesium deficiency has been increasingly studied for its potential role in various health conditions. Tooth grinding (bruxism) is a condition characterized by the grinding and/or clenching of teeth. While the causes of bruxism are multifactorial—including stress, anxiety, and misaligned teeth—research has explored the role of nutritional deficiencies in this condition.1
One such nutrient is magnesium, an essential mineral involved in more than 300 enzymatic reactions in the human body. Unfortunately, according to the World Health Organization in 2018, 75% of the US population is below the recommended daily allowance (RDA) for magnesium (310–420 mg daily).2
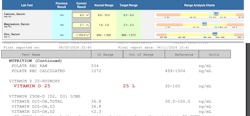
Signs of magnesium deficiency include muscle cramps/soreness, poor sleep, eyelid twitching, fatigue, poor blood sugar metabolism, irregular heartbeat, and mental conditions. Osteoporosis and bone fracture have also been associated with low magnesium as it is a cofactor needed for vitamin D uptake and can result in low vitamin D levels (figure 1).3
Teeth grinding and low magnesium
Lack of magnesium in the diet may also exacerbate bruxism by causing muscle hyperactivity, increased cortisol levels, and decreased sleep quality.4
- Muscle hyperactivity: One of the key findings is that magnesium deficiency may lead to muscle hyperactivity. Magnesium plays a crucial role in muscle contraction and relaxation. When magnesium levels are low, muscles—including those in the jaw—may become overactive, leading to increased instances of bruxism.
- Stress and neurotransmitter regulation: Magnesium also has a calming effect on the body by regulating neurotransmitters that control the release of stress hormones such as cortisol. High stress levels are a known trigger for bruxism. Therefore, maintaining adequate magnesium levels can help reduce stress and, consequently, teeth-grinding episodes.
- Improved sleep quality: Another significant finding is the impact of magnesium on sleep quality. Poor sleep is both a cause and a result of bruxism. Magnesium supplementation has been shown to improve sleep quality, thereby potentially reducing the occurrence of teeth grinding during sleep.
Implications for dental health-care providers
Magnesium supplementation: Given its role in muscle relaxation and stress reduction, magnesium could be a valuable addition to the treatment protocols for bruxism. Health-care providers could consider recommending magnesium supplements, especially for patients who exhibit signs of magnesium deficiency. Magnesium serum levels can be measured by lab blood tests or in-office devices. In general, magnesium supplements should be taken in smaller milligram amounts multiple times a day to increase absorption. Organic magnesium salts (such as magnesium glycinate, citrate, taurate, and malate) are better absorbed than inorganic magnesium salts (such as magnesium oxide).
Magnesium supplementation includes:
- Magnesium glycinate (readily absorbed by the body)—also known as bisglycinate—works on muscle relaxation, anxiety, insomnia, stress reduction, and lowers blood pressure (figure 2).
- Magnesium citrate (readily absorbed) lowers anxiety, depression, mood swings, and migraines.
- Magnesium taurate (readily absorbed) lowers blood sugar, improves insulin sensitivity, improves cardiovascular function, and is associated with antiaging practices.
- Magnesium threonate is better for brain function than muscle relaxation as it crosses the blood-brain barrier. Two grams of magnesium threonate has only 144–288 mg of magnesium, so it is not the best supplement for raising plasma magnesium.
- Magnesium chloride is better for skeletal muscle and alleviation of sore muscles.
- Magnesium oxide (poorly absorbed) is not advisable.
Dietary recommendations
Encouraging a diet rich in magnesium could also be beneficial. Foods high in magnesium—such as dark chocolate, avocados, nuts, legumes, tofu, seeds, fatty fish, bananas, and whole grains—should be incorporated into the diet of individuals prone to bruxism associated with magnesium deficiency.
Conclusion
By influencing muscle activity, stress levels, and sleep quality, magnesium supplementation plays a multifaceted role in the management of bruxism. Through addressing both the physiological and psychological triggers of bruxism, magnesium supplementation offers a holistic approach to treatment. Dental health-care providers should consider evaluating magnesium levels in patients presenting with bruxism/clenching, and recommend supplementation if deficiencies are found.
Since there is a lack of research in this area and most papers focusing on case reports, future research should concentrate on randomized clinical trials to further validate these relationships and explore optimal dosing strategies.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
References
- Lehvilä P. Bruxism and magnesium. Literature review and case reports. Proc Finn Dent Soc. 1974;70(6):217-224.
- Head K. Who is at risk for magnesium deficiency? Thorne Take 5 Daily. January 12, 2018. Accessed July 1, 2024. https://www.thorne.com/take-5-daily/article/who-is-at-risk-for-magnesium-deficiency
- Zittermann A. Magnesium deficit – overlooked cause of low vitamin D status? BMC Med.2013;11:229. doi:1186/1741-7015-11-229
- Grimaldi BL. The central role of magnesium deficiency in Tourette’s syndrome: causal relationships between magnesium deficiency, altered biochemical pathways and symptoms relating to Tourette’s syndrome and several reported comorbid conditions. Med Hypotheses. 2002;58(1):47-60. doi:10.1054/mehy.2001.1447
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.