Comparing popular wearable sleep tracking devices
Key Highlights
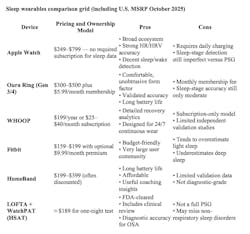
- Consumer sleep wearables like Apple Watch and Oura Ring offer valuable insights into sleep patterns but remain less accurate than clinical sleep studies (PSG and HSAT).
- Apple Watch and Oura Ring show the strongest validation for sleep and heart-rate tracking, while Fitbit provides good value and WHOOP focuses on recovery analytics.
- For patients with suspected sleep apnea, clinical testing such as a home sleep apnea test (HSAT) or full polysomnography (PSG) remains the diagnostic gold standard.
“My Fitbit says I sleep great. My wife doesn’t know what she’s talking about when she says she sees me stop breathing.”
“My Apple Watch says I sleep terrible, but I feel fine. It’s how I always sleep.”
“I feel like crap. I sleep like crap. My Oura Ring tells me I am crap. But what do I do about it?”
I hear stuff like this every day from dental patients we screen for sleep disordered breathing. Metrics matter. As a dentist and practice owner, I know that tracking our production, our collections, and our procedures is key to the health of the business. As I have learned, the numbers tell a story.
I love the advent of wearable health trackers and the awareness they’ve brought to a critical pillar of our health: sleep. Using actigraphy (movement) and photoplethosomnography (changes in blood volume in capillaries) to track heart rate, heart rate variability, and blood oxygen, many trackers use an algorithm to compute a sleep score and track deep and light sleep for the wearer.
But trackers don’t tell the rest of the story. Patients don’t know what to do with the information. Too many well-intentioned but ill-informed patients equate their sleep wearable to an actual diagnostic sleep study. Questions remain regarding the accuracy, reliability, and clinical utility of these consumer-grade devices. While manufacturers claim advanced algorithms and high precision, independent studies have shown mixed results when compared with gold-standard sleep measurement methods. That’s what we’ll dive into with the rest of this article: the current capabilities, limitations, and implications of wearable sleep trackers.
If the numbers tell a story, what are they saying about you and your sleep?
Additional reading: A new pill to treat sleep apnea
Top 5 sleep devices
Apple Watch: Apple has reported internal validation of its sleep stage classifier, and multiple independent studies have examined physiologic signals such as HRV. A 2024 peer-reviewed study found Apple Watch Series 9/Ultra 2 HRV closely tracked a Polar H10 chest strap reference, supporting reliable autonomic signal capture that underpins sleep algorithms.1 Apple’s technical white paper details design/validation for its sleep staging classifier.2 Recent independent testing also suggests strong heart-rate and respectable sleep-stage agreement versus reference devices.
Oura Ring: Multiple peer-reviewed and independent validations show solid sleep detection and moderate stage classification.3 A 2024 study of Gen3 reported high reliability with stage-specific accuracies (REM up to ~91%), and Oura has publicized comparative results (Cohen’s κ ~0.65 for four-stage classification), outperforming Apple and Fitbit4 in that analysis.5 Other datasets show mid-50% to high-70% stage accuracy depending on methods and comparators—typical for consumer devices.6
WHOOP: Recent peer-reviewed work indicates acceptable accuracy for sleep/cardiac variables for cohort tracking; frequent wear improves day-to-day reliability.7 (Quality can vary across firmware and model generations.)
Fitbit: Reviews and meta-analyses report good detection of sleep versus wake and total sleep time, with moderate accuracy for stages (often overestimating light sleep and underestimating deep sleep).
HumeBand: This newer device emphasizes “metabolic capacity” and AI guidance. As of now, public validation appears limited to marketing claims and tech-media reviews; peer-reviewed sleep-staging validation is sparse, so clinicians should consider it emerging/experimental for sleep staging versus PSG.
How do sleep device wearables compare with PSG and HSATs?
Formal polysomnography (PSG) remains the gold standard for sleep staging and sleep disorder diagnosis (EEG, EOG, EMG, ECG/respiratory channels). HSATs (e.g., WatchPAT) provide clinically relevant respiratory metrics (AHI, oxygen saturation, etc.) at home and are suitable for diagnosing obstructive sleep apnea in appropriate patients, though they do not comprehensively stage sleep like PSG.8 Johns Hopkins and Mayo Clinic emphasize that HSATs are simplified compared to PSG but are practical, lower-cost diagnostic pathways for suspected OSA.9
WatchPAT (Itamar/ZOLL) uses peripheral arterial tonometry with oximetry and actigraphy to infer respiratory events and sleep stages; multiple studies show good correlation with PSG for AHI and clinically useful differentiation10 (e.g., REM-related OSA, central versus obstructive features).
SleepVibe is the first sleep aid that uses nonaudible binaural beats. Unlike traditional aids that rely on sound, SleepVibe is silent, using a low-frequency magnetic field to deliver binaural beats. The technology is designed to support the brain's natural sleep patterns, gently helping to promote a deep, restorative sleep. SleepVibe has been safety tested by an FDA-approved lab. Many people report increased deep and REM sleep using Oura and Fitbit. There are no peer-reviewed studies available but there is current research pending.
Conclusion
Consumer wearables can estimate total sleep time and broad sleep patterns reasonably well, but they still trail formal polysomnography (PSG) for staging and for diagnosing sleep disorders. Among mainstream wearables with recent validation, Apple Watch and Oura Ring tend to perform best overall on sleep metrics; Fitbit offers strong value with modest accuracy; WHOOP is competitive for recovery trends but requires a subscription; HumeBand is emerging but has limited peer-reviewed validation to date. For diagnosis of sleep apnea, a home sleep apnea test (HSAT) such as WatchPAT—offered by LOFTA—is the appropriate consumer-first pathway, with better alignment to clinical endpoints than lifestyle wearables.
Takeaways
- For sleep optimization, Apple Watch or Oura Ring are the most validated consumer options.
- For suspected sleep apnea, recommend HSAT (e.g., WatchPAT via LOFTA) or PSG.
- Wearables are suitable for behavioral guidance and trend tracking, not diagnosis.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
References
- O’GradyB, Lambe R, Baldwin M, Acheson T, Doherty C. Validity of Apple Watch Series 9 and Ultra 2 for serial measurement of heart rate variability and resting heart rate. Sensors. 2024;24(9):6220. doi:3390/s24196220
- Apple Inc. Estimating sleep stages from Apple Watch. Apple Technical White Paper. September 2023. https://www.apple.com/healthcare/docs/site/Estimating_
Sleep_Stages_from_Apple_Watch_Sept_2023.pdf - Svensson T, Madhawa K, Nt H, Chung UI, Svensson AK. Validity and reliability of the Oura Ring Generation 3 (Gen3) with Oura sleep staging algorithm 2.0 (OSSA 2.0) when compared to multi-night ambulatory polysomnography: a validation study of 96 participants and 421,045 epochs. Sleep Med. 2024;115:251-263. doi:10.1016/j.sleep.2024.01.020
- Schyvens AM, Van Oost NC, Aerts JM, et al. Accuracy of Fitbit Charge 4, Garmin Vivosmart 4, and WHOOP versus polysomnography: systematic review. JMIR mHealth and uHealth. 2024;12:e52192. doi:10.2196/52192
- Robbins R, Weaver MD, Sullivan JP, et al. Accuracy of three commercial wearable devices for sleep tracking in healthy adults. Sensors (Basil). 2024;24(20):6532. doi:10.3390/s24206532
- Park JE, Ahn EK, Yoon K, Kim J. Performance of Fitbit devices as tools for assessing sleep patterns and associated factors. J Sleep Med. 2024;21(2):59-64. doi:13078/jsm.240010
- Grosicki GJ, et al. WHOOP measures validated vs ECG/PSG; adherence effects. Sports. 2025;13.
- Dobbin ML, Bernard A, Pyle L, et al. Comparison of WatchPAT to polysomnography measurement of apnea-hypopnea index and obstructive sleep apnea severity in adolescents with overweight and obesity. J Clin Sleep Med. 2025. Published online April 1, 2025. doi:5664/jcsm.11530
- Johns Hopkins Medicine. What to know about an at-home sleep test. Johns Hopkins Health Library, 2025. https://www.hopkinsmedicine.org/health/wellness-and-prevention/what-to-know-about-an-at-home-sleep-test
- LOFTA. At-home sleep apnea test pricing and WatchPAT workflow. LOFTA Inc., 2025. https://lofta.com/products/sleep-apnea-test
About the Author
Erin Elliott, DDS
Erin Elliott, DDS, grew up in southern California but went away to a small NAIA school in western New York where she played collegiate soccer and graduated summa cum laude from Houghton College. After graduating from Creighton Dental School in 2003, she settled in north Idaho to begin her general dentistry career. She has a special interest in dental sleep medicine and has lectured extensively on this topic. Dr. Elliott is an active member of various dental associations, including the American Academy of Sleep Medicine and American Academy of Dental Sleep Medicine. She is the past president and a diplomate of the American Sleep and Breathing Academy. She teaches a two-day sleep apnea implementation course with 3D Dentists and Tarun Agarwal, DDS.

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.