Is it time to retire the free gingival graft procedure in light of new alternative tissue grafting materials?
The free gingival graft (FGG) is a surgical procedure frequently used in periodontics to increase the amount of keratinized tissue surrounding a tooth or a dental implant. Keratinized tissue plays a major role (around teeth and dental implants), helping to maintain and facilitate oral hygiene. Dr. Nabers introduced this surgical technique almost 50 years ago in 1966.
ALSO BY DR. ALESSANDRO GEMINIANI |How to increase safety and reduce complications during sinus lift
Fig. 1: Initial situation, before free gingival graft. Note the lack of gingiva buccal to teeth Nos. 24 and 25.
Fig. 2: Follow-up at eight weeks. The free gingival graft was successful in increasing the amount of gingival adjacent to teeth Nos. 24 and 25.
Indications for free gingival graft
- Increase of keratinized tissue adjacent to teeth, dental implants, or edentulous ridges
- Coverage of certain type of gingival recessions
Contraindications for free gingival graft
- High esthetic demand
- Need for an intraoral donor site
ALSO BY DR. ALESSANDRO GEMINIANI |And you thought dental plaque was bad: preventing evolution of biofilms
The esthetic result of the free gingival graft technique can range from very poor to excellent, depending on tissue characteristics proper of each patient. As this is not always predictable, I tend not to use this technique in patients demanding an excellent esthetic outcome. However, a modification to the original technique, recently published by Dr. Cortellini and colleagues (partly epithelialized free gingival graft, 2012), seems to overcome this limitation. The second major limitation is the need for a donor site. Most commonly the tissue is harvested from the palate. The need for a second surgical site may increase the length of the procedure, as well as postoperative discomfort. Protecting the area with a stent or a periodontal dressing can reduce the discomfort.
Fig. 3: The stent protects the donor site, increasing the postoperative comfort.
I like to use a vacuum-form stent. To fabricate the stent, you can use a thermoplastic material (the same used for bleaching trays) that is vacuum-pressed on the preoperative dental cast. This way the patient can use this thin appliance to protect the wound. The stent fits tightly and does not alter the speech too much.
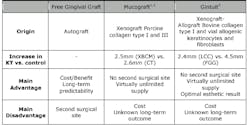
Recently, alternative grafting materials have been introduced into the market to avoid harvesting tissue from the palate. The FDA has approved two grafting materials with similar indications to a free gingival graft: a xenogenic bioabsorbable collagen matrix (XBCM) (Mucograft by Osteohealth) and a living cellular construct (LCC) (by Organogenesis).
Table 1: Brief comparison of advantages and disadvantages of free gingival graft and alternative techniques.
KT= keratinized tissue; FGG= free gingival graft; CT= subepithelial connective tissue graft; XBCM= Mucograft; LCC= Gintuit.
Compiled from:
1. Sanz M et al. Clinical evaluation of a new collagen matrix (Mucograft prototype) to enhance the width of keratinized tissue in patients with fixed prosthetic restorations: a randomized prospective clinical trial. J Clin Periodontol 2009;36(10):868-876.
2. Lorenzo R et al. Clinical efficacy of a xenogeneic collagen matrix in augmenting keratinized mucosa around implants: a randomized controlled prospective clinical trial. Clin Oral Implants Res 2012;23(3):316-324.
3. McGuire MK et al. Living cellular construct for increasing the width of keratinized gingiva: results from a randomized, within-patient, controlled trial. J Periodontol 2011;82(10):1414-1423.
Fig. 4: Split mouth trial, free gingival graft vs. Gintuit. (From Gintuit website)
In conclusion, I do not think it is time to retire the free gingival graft procedure, at least not yet. The alternative grafting materials (such as Gintuit and Mucograft) offer unique advantages (i.e., no need for a donor site, virtually unlimited supply, reduced surgical time, etc.) but lack in long-term follow up. In the near future, progress in the development of these materials and reduced manufacturing costs can make the free gingival graft an obsolete technique. I am interested in the developments of the living cell construct (Gintuit) as it offers a natural-looking outcome, which is an advantage in the treatment of patients who demand highly esthetic results.
Fig. 5: Free gingival graft 30 years follow up — (a) before, (b) after. (From Pini Prato et al, 2012)