ADDITIONAL READING |Diagnosing between ailing and failing implants: The haste to remove salvageable implants
The possible etiologies of EIBL were described in an article by Tatarakus et al. in Implant Dentistry in 2012. They list the six possible etiologies as:
1. Surgical trauma
2. Establishment of biologic width
3. Presence of a microgap
4. Peri-implantitis
5. Occlusal overload
6. Implant crest module
To this list, based on the literature, Dr. Paul Rosen and I have added micromotion of the prosthetic/abutment interface, early implant exposure in a two-stage implant placement protocol, and poor implant position. All of the above, with the exception of establishment of biologic width, can be avoided with attention to proper implant placement by following the manufacturers’ guidelines, use of computerized cone beam scans prior to placement, as well as a surgical guide made from an ideal wax-up. Restorative procedures should mimic those used with natural teeth with proper crown fit and occlusion of the implant-supported restorations. Prosthetic parts should be matched not mixed to the type of implant placed.
The possible causes of late implant bone loss include:
1. Implant overload
2. Parafunction
3. Poor implant placement
4. Cranial growth and development
5. Peri-implantitis
The latter has been shown in two recent systematic reviews of literature to have a prevalence of approximately 10% of all implants and 20% of patients after an implant has been in function for five to 10 years. According to statistics from two independent research companies, this would mean that more than 1.2 million implants placed in the United States alone over the last five years have bone loss resulting from peri-implantitis.
ADDITIONAL READING |Restoration of a damaged dental implant due to removal of a fractured screw: thinking outside the box
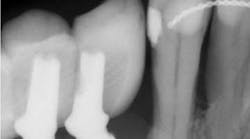
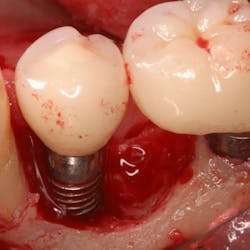
The diagnosis and prevention of peri-implantitis was described in detail in a paper published in the Journal of Periodontology in 2013. It states that peri-implantitis is characterized by inflammation in the tissue surrounding the implant, bleeding on probing (BoP), and radiographic evidence of bone loss exceeding 1.5 mm (due to biologic width formation) and greater than 0.2 mm per year after that. The best treatment is prevention, and it is the responsibility of the hygienist and restorative dentist to examine each implant at maintenance visits. If signs of peri-implantitis exist, early treatment has been shown to prevent further bone loss and restore the implant to health. Radiographs should be taken immediately on the day of restoration and then periodically whenever BoP is evidenced with probing depth increases. Treatment of moderate or advanced peri-implantitis with bone loss up to two-thirds of the implant length has been shown to be successful in restoring lost bone support following a published regenerative procedure (See Froum SJ, et al. Successful management of peri-implantitis with a regenerative approach: a consecutive series of 51 treated implants with 3- to 7.5-year follow-up. Int J Periodontics Restorative Dent. 2012.).
The key to any successful maintenance program, as well as treatment, is a thorough decontamination of the biofilm on the diseased implant surface. Special tools specific for this with the use of air-powder devices and chemical application (i.e., minocycline 50 mg) followed by copious irrigation with saline, if performed diligently, is essential to prevent and help restore peri-implant bone loss.
Editor’s note: For more information on techniques to identify, prevent, and treat peri-implant bone loss, read the second edition of “Dental Implant Complications,” edited by Dr. Stuart Froum, to be published in the fall of 2015. You are also invited to attend the Dental Implant Complication Symposium on December 8 in Fort Lauderdale, Florida, where Drs. Stuart J. Froum and Paul Rosen will present a complete review of the topic of peri-implant bone loss with the most effective methods of diagnosis and treatment described in detail.
ALSO BY DR. STUART FROUM |My patient's implant is bleeding; what do I do?