Periocclusion
Periodontal treatments are now well documented and codified. It is now undisputed that nonsurgical treatment needs to remove the largest amount of periodontal pathogens as possible in order to limit the individual inflammatory response and prevent future bone loss. Supragingival decontamination is ensured by the patient’s daily oral hygiene habits, and the dental team performs the infra-gingival decontamination by scaling and root planing.
RELATED |Dental implant therapy in the future
Nevertheless, some patients present with so-called aggressive periodontitis, which is a severe and rapid-paced form of periodontal disease due to some now more understood risk factors. The most obvious of those risk factors include smoking, diabetes, and genetic predisposition. But as long as periodontists are not specifically trained in occlusion, the relationship between periodontal disease and occlusion risk factors has never been clearly demonstrated nor systematically taken into account for the treatment of periodontal patients.
RELATED |'My implant is too shallow and now I'm getting food stuck between my teeth'
The clinical case presented here is a 30-year-old young woman with no medical condition and a nonsmoker. Her chief complaints are tooth mobility and gingival bleeding.
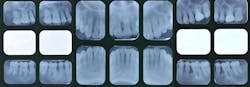
Fig. 1: Radiographic status of a 30-year-old Caucasian female
The clinical examination shows:
- Periodontal examination: The patient has very good oral hygiene, 6 mm to 9 mm pockets, bleeding on probing, and tooth mobility (especially tooth No. 4).
- Dental examination: Tooth No. 14 has been endodontically treated and now holds a PFM crown. Tooth No. 3 holds two tiny alloys.
- Functional examination: The patient reports no musculo-articular symptoms though lateral jaw movements exhibit working-side interferences on the premolars.
- Esthetic examination: The patient reports no symptoms.
Diagnosis for this patient is an aggressive periodontal disease. The important periodontal bone loss is due to the combination of three risk factors:
- Presence of periodontal pathogens
- Genetic predispositions
- Poor repartition of occluso-functional stress
Prognosis is poor for teeth Nos. 4, 12, and 15.
Fig. 2: Important bone loss around tooth No. 4
Treatment planning for this patient is:
- Oral hygiene instruction and reinforcement
- Full-mouth decontamination: scaling and root planing associated with local antibiotics (Parocline®)
- Reevaluation three months postop
- Occlusal equilibration
- Long-term maintenance
Twelve months after initial therapy, the patient’s plaque control is excellent and she no longer reports tooth mobility or gingival bleeding.
Fig. 3: 12 months after initial therapy
Tooth No. 4, because of its excessive bone loss, is further investigated. Probing is now normal (1.5 mm) — no bleeding, which indicates a gingival reattachment. This particular tooth mobility has improved from 4 to 2.
Fig. 4: Probing around tooth No. 4: 1.5 mm and no bleeding
The occlusal equilibration has been performed in order to get the maxillary premolars out of the way during mandibular eccentric movement while maintaining intercuspation contacts on the palatal cusps. The patient immediately felt an improvement of her bite.
Fig. 5: The occlusal equilibration consisted in unloading tooth No. 4 during the lateral excursion of the lower jaw and now enables a canine guidance
Fig. 6: Radiographic aspect of tooth No. 4 12 months after treatment. Note the bone regeneration.
The patient now follows a six-month recare program.
So far, this case has been successful because of positive influences:
- The patient’s young age
- Her positive and motivated mindset
- An efficient decontamination protocol
- A functional analysis of the occlusal relationships
- A long-term maintenance
Occlusion is the field of dentistry that lacks the most scientific evidence because:
- Occlusal physiology and pathology, such as trauma, are difficult to define and agree on.
- Occlusal pathology is often multifactorial so the studies’ designs are altered by bias.
As a result, there is very little evidence of a statistical relationship between occlusion and periodontal disease. Yet, some very careful clinicians have noticed that unbalanced occlusal stress could trigger severe bone loss on a weak periodontium. For those practitioners, periodontal treatment is always part of a comprehensive and multidisciplinary treatment plan whose ultimate goal is oral function. We should always keep in mind that we cannot stabilize a dentition without creating the conditions for its harmonious function. That is also why functional examination of our patients should be systematic.
Periodontal therapy needs to focus on three core elements:
- The patient’s medical condition
- Microbiological status
- Functional overloads on teeth
Recommended reading
- Hallmon WW. Occlusal trauma: effect and impact on the periodontium. Ann Periodontol 1999; 4:102-108.
- Kinane DF. Periodontitis modified by systemic factors. Ann Periodontol 1999; 4:54-56.