Nonsurgical endodontic retreatment with the aid of cone beam (CBCT) imaging
Endodontic therapy under current treatment protocol shows long-term clinical success rates of 86% to 92%. Even with the high clinical success rate of initial endodontic treatment, it’s obvious to see this leaves clinicians with a 14% incidence (on the high side) of encountering post-treatment disease in our patient population. Some common causes of post-treatment disease include persistent or reintroduced intraradicular microorganisms, extraradicular infection, foreign body reaction, and true cysts. There are a multitude of reasons for any of the above clinical situations to arise.
The question that we as clinicians are left to answer through radiographic imaging and clinical testing are first, what is the etiology, and second, what is the prognosis of any suggested treatment. Two-dimensional radiographs have aided in diagnosis of dental disease for many years, with the first dental radiograph claiming to be taken in 1896. But as with all technology, it has its limitations. When reviewing cases for nonsurgical retreatment, surgical retreatment (apicoectomy), or extraction, I like to have all of the information currently available to me. In my office I will routinely take a narrow-field CBCT image of any teeth exhibiting post-treatment disease. Presented in the article will be a case that was treated with the aid of CBCT imaging and a surgical operating microscope.
ADDITIONAL READING |Endodontic therapy vs. implant maintenance: an evidence-based review
Case No. 1
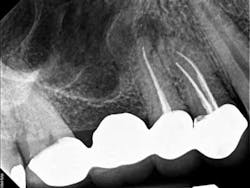
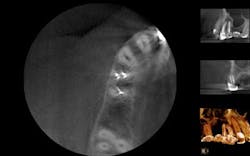
A 50-year-old male presented to my office on referral from his general dentist for evaluation of a large, periapical radiolucency relating to Nos. 4 and 5. Appropriate bitewing and peri-apical radiographs were taken (Fig. 1) for initial evaluation. After all clinical testing was performed, the recommendation was made to take a narrow-field CBCT image of teeth Nos. 4 and 5 (Figs. 2 and 3). The axial view reveals an untreated buccal canal on tooth No. 4 and potential separated instruments in both the buccal and palatal canal space of No. 5. Tooth No. 5 (Fig. 3) shows a short fill, meaning the entire canal space may not have been properly shaped and cleaned. With the three-dimensional images, we now have a better understanding of why these teeth present with post-treatment disease. This information is extremely important when discussing etiology and prognosis with our patients. It will also financially benefit the patient to maintain his existing fixed prosthesis with conservative retreatment of Nos. 4 and 5, knowing that we should have a high degree of long-term success seeing a clear etiology of the post-treatment disease.
ADDITIONAL READING |Dismay with kid decay: treatment options for broken down permanent teeth in the mixed dentition
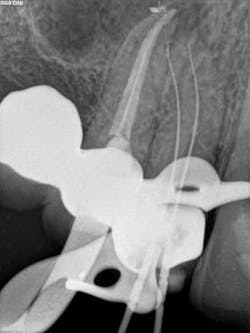
The patient was appointed to start NSRCT retreatment on tooth Nos. 4 and 5. Upon the initial visit after proper anesthesia and rubber dam isolation, the teeth were treated using a surgical operating microscope. Conservative access was gained through the occlusal of No. 4, the untreated buccal canal was located and treated, and the palatal canal presented with a gutta percha fill. The palatal canal was retreated and both canals where packed with Ca(OH)2 paste for 10 days. At the patient’s next visit, No. 4 remained asymptomatic. After proper irrigation and additional cleaning and shaping, No. 4 was obturated and a coronal seal placed at this appointment. Endodontic therapy is not complete until we have coronally sealed the tooth. Tooth No. 5 was accessed after the obturation of No. 4, and it was noted that the metallic-like images we had noted on the CBCT scan were indeed Thermafil metal carriers. Each carrier was isolated under the microsope and removed in a similar fashion to the removal of a separated instrument (Fig. 4). After proper cleaning and shaping, No. 5 was packed with an interappointment Ca(OH)2 dressing, and the patient was appointed for completion of No. 5.
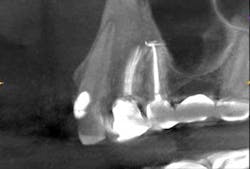
Ten days later, the patient returned asymptomatic. Again, after proper anesthesia and isolation the temp filling was removed, additional irrigation, along with cleaning and shaping of the canals was continued, the case was obturated, and a permanent seal placed that day. The patient reported for a 14-month follow-up and a subsequent CBCT image was obtained (Fig. 7). The sagittal view shows complete boney healing of the previous periapical lesion, and retention of the fixed prosthesis.
Discussion
After proper diagnosis and testing along with CBCT imaging, a treatment plan for the patient was decided upon with input from both the patient and his general dentist. I believe that the treatment plan we decided upon was both minimally invasive and cost-effective for our patient, with a high potential for long-term success. The patient is due for a two-year recall where traditional 2-D images will be taken. The patient was informed that due to the size of the lesion apical surgery may also be needed, but based on the healing after only 14 months, it does not seem that any additional procedures will be needed to maintain the fixed prosthesis.
Fig. 3: CBCT sagittal view
Fig. 4: Metal carriers removed
Fig. 5: No. 4 filled; No. 5 file shot
Fig. 6: Immediate postop Nos. 4 and 5 after removal of metal carriers
Fig. 7: CBCT sagittal view (Nos. 4 and 5) 14-month postop, showing complete resolution of the apical lesion with intact lamina dura