Biomimetic technology: putting the tooth fairy out of business
As a dental practitioner, how many times has a patient said to you during the course of fabricating a treatment plan, “Well, if this were your mouth and your tooth, what would you do?”
It’s a rational question that may not get proper consideration especially when a decision is being made whether to extract a tooth and place an implant vs. trying to regenerate the periodontium. This question is further complicated by the advancements in technology that give us as practitioners an increased ability to regenerate lost tissue and change the prognosis of teeth … teeth that may have been deemed questionable to hopeless may now be re-allocated to the category of fair or guarded (depending on the classification system you use). Of course, recent literature has demonstrated that implants are not without their associated problems and teeth may be easier to “save” when they have lost hard and soft tissue. (1)
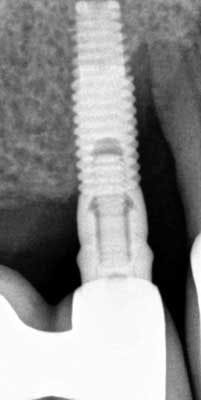
The following is a case example of a patient who presented with an ailing implant No. 5 diagnosed with advanced peri-implantitis. Tooth No. 6 was also involved with severe periodontitis. An argument could have been made to extract both the implant and the tooth and try to replace the area with another two implants after grafting or a fixed partial denture. Both options may have left the patient with severe ridge defect that would have needed to be treated with either pink ceramic or multiple attempts at regeneration. With new, improved biomimetic technology, both the implant and the tooth were saved.
ALSO BY DR. JENNIFER HIRSCH DOOBROW | Emdogain: a game changer
This is a 62-year-old African American male with a medical history positive for GERD. He takes Nexium. He was referred for an ailing implant No. 5 with a PD of 15+ mm as well as a PD of 15+mm on adjacent natural tooth No. 6. Upon initial presentation, suppuration exuded from the sulcus of No. 5i and No. 6. The surgery was as follows:
- Intrasulcular incisions
- A full thickness flap was reflected
- Thorough debrided and degranulation with hand instrumentation and a Cavitron
- Cortical-cancellous allograft was mixed with enamel matrix derivative for 15 minutes
- A tetracycline slurry was used for chemical conditioning of the tooth and the implant surface for approximately two minutes, and then thoroughly irrigated with saline rinses
- EDTA 24% was placed on both implant and tooth and allowed to sit for four minutes, rinsed, and dried with nonwoven gauze
- Enamel matrix derivative was added to the base of the alveolar defect on tooth No.6 and implant No. 5
- A combination of allograft and enamel matrix derivative was placed into both defects
- 4-0 vicryl vertical mattress sutures were used to coronally advance the tissue along with simple interrupted sutures
- Postop: Patient placed on CHX rinse for two weeks, and no additional oral hygiene aides for two weeks
- Patient was seen two weeks postop and a review of OHI occurred
- Patient returned for two follow-up appointments and then was noncompliant for one year
- Patient presented back to our office with 3-4 mm probing depth and now has a stable result for not only the tooth but also the implant
The addition of a biologic agent in addition to a cortical cancellous allograft allowed me not only to build back the foundation around a natural tooth, but also an ailing implant. Think about it — what would you rather have a tooth or an implant in your mouth or under your pillow?
Intraoperative photo
2-year postop radiograph with PD 3-4 mm around No. 5 implant and No. 6 natural tooth
Reference
1. Levin et al. JADA. Oct. 2013;144(10):1119-1133.