Restoration of a damaged dental implant due to removal of a fractured screw: thinking outside the box
Dental implant success has been well documented in the literature (1); however, failure does occur. (2) Typically, failure can be categorized as either early or late. Early failure occurs prior to the implant integrating, with causes such as overheating during osteotomy preparation, overpreparation of the osteotomy, implant contamination during surgery, poor bone quality, lack of primary stability, and macro/micro motion. The etiology of late failure is most often either related to a bacterial event (3) such as peri-implantitis and/or biomechanical failure due to occlusal trauma and/or implant overload. (4)
ALSO BY DR. SCOTT FROUM |An alternative to conventional dental implants: short implants
Failure, as it relates to biomechanical issues, is often due to off-angled forces and/or overload on an implant fixture mixed with time. Fatigue of the implant material is often cumulative; certain breakdowns often happen along the way until catastrophic failure occurs (implant fracture). The first sign — “tell” if you are a poker player — of occlusal disharmony is usually the screw loosening. Most often the dentist will tighten the screw and think the problem is solved until loosening occurs again. After this exercise in futility is repeated without addressing the problem of occlusal dysfunction, the screw can ultimately break. Breakage of a screw in an implant fixture can present a complicated situation as the ease of screw removal often depends on the apical-coronal location of the fracture. The following case highlights a unique method of implant restoration when damage occurs to the implant fixture due to the attempted removal of a fractured screw.
ALSO BY DR. SCOTT FROUM |A new tool in the fight against peri-implant disease
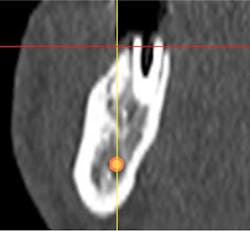
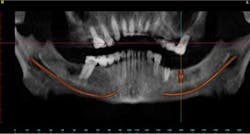
Case study A 58-year-old male with a noncontributory medical history presented to a private practice for a complete rehabilitation of his dentition due to years of bruxism and parafunction. (Fig. 1) After surgical and restorative consultations, a treatment plan was fabricated. The treatment plan included restoring his lost vertical dimension, restoring his natural dentition with porcelain-fused-to-metal full-coverage crowns, and replacing his lost posterior teeth with dental implants. After his vertical dimension was restored with an acrylic bite plate to a position harmonious with TMJ function, crown-lengthening surgery was performed. (Fig. 2)Fig. 2 Six weeks after, the teeth were temporized to develop soft tissue margins/interdental papillae. (Figs. 3 and 3a) The patient was kept in temporaries for three months, during which time an implant was placed in site No. 19. Both the natural dentition and the implant were completed at the same time, three months after implant placement. (Fig. 4) Because of the patient’s occlusal issues, the implant was screw-retained, and the patient was given a maxillary night guard. Three weeks after insertion, the patient presented with a loose abutment screw. The dentist tightened the screw and sent the patient home. This cycle was repeated two more times until the patient presented again with a loose crown, but this time, a fracture implant screw. The dentist attempted to remove the screw with a Cavitron and drilling the implant screw out to release preload, but to no avail. The case was then referred to my office for implant removal.
Fig. 3a
Fig. 5
Fig. 6
Fig. 7
Fig. 8
References
1. Esposito H, Lekholm T. Biological factors contributing to failures of osseointegrated oral implants I. Success criteria and epidemiology. Eur J Oral Sci 1998;106:521-557.
2. Karoussis IK, Müller S, Salvi GE, Heitz-Mayfield LJ, Brägger U, Lang NP. Association between periodontal and peri-implant conditions: a 10-year prospective study. Clinical Oral Implants Research 2004;15:1-7.
3. Mombelli A, van Oosten MA, Schurch E, Lang NP. The microbiota associated with successful or failing osseointegration titanium implants. Oral Microbiology and Immunology. 1987;2: 145-151.
4. Brunski JB. Biomechanical factors affecting the bone-dental implant interface. Clin. Materials 1992;10:153-201.