Are we there yet? A new instrument that determines when dental implants are ready to be restored
Dr. Scott Froum says osseointegration of dental implants is dependent on a variety of patient-related factors, and because each patient heals differently, load time is different. He explains how using resonance frequency analysis (RFA) to measure implant stability is a simple, fast, noninvasive way to test maturity of bone around the implant without exposing patients to radiation.
Although dental implants enjoy a high survival rate, a percentage of implants fail for a variety of reasons. (1) Patient-related factors—such as medical history, medications, history of periodontal disease, occlusal interferences, parafunction, and social factors (e.g., smoking status)—play a role in determining the percentage of implant failure. (2) Local anatomic factors, such as bone quality and quantity, determine variations of therapy, such as timing of fixture placement and restorative loading. (3) In the early days of implant treatment, the miracle of osseointegration was appreciated by edentulous patients, and a typical protocol of waiting six to nine months for integration after placement was tolerated. As research in implant science evolved, immediate placement/loading protocols became viable options, since they enjoyed similar success rates as conventional submersion protocols. As the time from placement to load decreased, the questions from implant patients of “Is my implant ready yet?” increased. Another common question patients may ask is, "Why is this taking so long when my friend got a tooth immediately?” These questions resulted in the invention of diagnostic tools capable of measuring when an implant is ready to load.
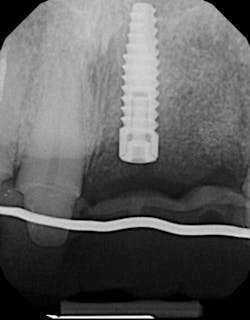
There are many different methods clinicians use to measure the maturity of the bone around the dental implant. Bone-to-implant contact is one measure of determining when implants are ready to load. Intraoral/panoramic radiographs, cone beam computed tomography (CBCT), microcomputed tomography (MCT), reverse torque testing, and resonance frequency analysis (RFA) are all methods that have been documented in the literature. The ability of standard imaging techniques, such as periapical and panoramic radiography, to measure bone-to-implant contact and integration levels have been questioned since standard imaging lacks the sensitivity needed for accurate assessment. (4) These two-dimensional radiographs may show bone surrounding an implant even when bone-to-implant contact levels are low (figure 1).
CBCT and MCT have been shown to be more sensitive than standard imaging at measuring bone mineral density, bone-to-implant contact, and maturity levels of bone around dental implants. (5) Different imaging systems have different conversion errors, and standardization of Hounsfield units and Grey values should not be made when comparing different scanners. (6) In other words, the image density around implants of scans taken by different systems may mean different things. (7) In addition, artifact and scatter around the dental implant may preclude an attempt at measuring implant stability (figure 2). The reverse torque test works by means of a specified reverse force placed upon the dental implant as a means of testing integration. This method is often invasive and can result in implant explantation if not carefully utilized. (8)
A better method of measuring implant stability and bone-to-implant contact that is noninvasive uses resonance frequency analysis (RFA) to determine the implant stability quotient (ISQ). RFA involves sending magnetic pulses to a small metal rod temporarily attached to the implant. As the rod vibrates, the probe reads its resonance frequency and translates it into an ISQ value. The clinical range of ISQ is normally in the 55 to 80 range. Higher values are generally observed in the mandible rather than in the maxilla. The higher the ISQ value, the higher the stability of the implant. (9) High stability means an ISQ value greater than 70; a value in the 60 to 69 range indicates medium stability; and an ISQ value less than 60 is considered to be low stability. Although this instrument was developed for research purposes, it has become very useful in the clinical environment. (10) After initial placement, a drop in ISQ levels can be expected during the healing phase. If this drop is large, usually more than 10% of the initial reading, it could signal that the implant is not healing well. (11)
The technical application of this instrument is extremely simple and expedient. New designs have also made RFA instruments easier to use. Older RFA instruments (Ostell) have a cord that connects to the digital readout, many toggle buttons, and a single-use-only peg that inserts into the implant. Newer instruments (PenguinRFA) use a cordless instrument and a multiuse peg that can be sterilized. The button is turned on and the instrument is held close to the peg. Within seconds, you have an ISQ reading (figures 3a and 3b).
Osseointegration is dependent on a variety of patient-related factors, and because each patient heals differently, the time to load is different. Two-dimensional imaging is unreliable and three-dimensional imaging can be obscure. Using RFA to measure an implant’s ISQ is a simple, fast, noninvasive means of testing maturity without exposing patients to radiation. The next time a patient asks you, "Are we there yet?" calmly reply, "Let me ask the penguin."
References
1. Muddugangadhar BC, Amarnath GS, Sonika R, Chheda PS, Garg A. Meta-analysis of failure and survival rate of implant-supported single crowns, fixed partial denture, and implant tooth-supported prostheses. J of Int Oral Health. 2015;7(9):11-17.
2. Salah S, Baroudi K, Nassani MZ. Factors associated with early and late failure of dental implants. J Investig Clin Dent. 2012;3(4):258-261. doi: 10.1111/j.2041-1626.2012.00162.x.
3. Friberg B, Jemt T, Lekholm U. Early failures in 4,641 consecutively placed Brånemark dental implants: a study from stage 1 surgery to the connection of completed prostheses. Int J Oral Maxillofac Implants. 1991;6(2):142-146.
4. Ritter L, Elger MC, Rothamel D, et al. Accuracy of peri-implant bone evaluation using cone beam CT, digital intra-oral radiographs and histology. Dentomaxillofac Radiol. 2014;43(6):20130088. doi: 10.1259/dmfr.20130088.
5. Bernhardt R, Kuhlisch E, Schulz MC, Eckelt U, Stadlinger B. Comparison of bone-implant contact and bone-implant volume between 2D-histological sections and 3D-SRμCT slices. Eur Cell Mater. 2012;23:237-247.
6. Kim DG. Can dental cone beam computed tomography assess bone mineral density? J Bone Metab. 2014;21(2):117-126. doi: 10.11005/jbm.2014.21.2.117.
7. Liu S, Broucek J, Virdi AS, Sumner DR. Limitations of using micro-computed tomography to predict bone–implant contact and mechanical fixation. J Microsc. 2012;245:(1):34-42. doi: 10.1111/j.1365-2818.2011.03541.x.
8. Jividen G Jr, Misch CE. Reverse torque testing and early loading failures: help or hindrance? J Oral Implantol. 2000;26(2):82-90.
9. Meredith N, Alleyne D, Cawley P. Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin Oral Implants Res. 1996;7(3):261-267.
10. Monje A, Ortega-Oller I, Galindo-Moreno P, et al. Sensitivity of resonance frequency analysis for detecting early implant failure: a case-control study. Int J Oral Maxillofac Implants. 2014;29(2):456-461. doi: 10.11607/jomi.3357.
11. Capparé P, Vinci R, Di Stefano DA, et al. Correlation between initial BIC and the insertion torque/depth integral recorded with an instantaneous torque‐measuring implant motor: an in vivo study. Clin Implant Dent Relat Res. 2015;17(Suppl 2):e613-e620. doi: 10.1111/cid.12294.
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.