GINGIVAL RECESSION is a common condition resulting from periodontal disease and mechanical trauma, among other causes. (1) By age 60, about 90% of Americans will have at least one site with ≥1 mm of recession, while about 40% will have at least one site with ≥3 mm of recession. (1) Sites with recession are likely to progress. (1) Esthetic concerns, dentinal hypersensitivity, prevention of caries and noncarious cervical lesions necessitate the treatment of gingival recession. (1) Multiple treatment options exist for the correction of gingival recession; however, the subepithelial connective tissue graft (SECT graft) continues to be considered the gold standard of gingival recession and soft-tissue grafting. (2)
Periapical pathology associated with pulpal necrosis, secondary to dental caries, is another condition seen quite frequently. Radicular (periapical) cysts are the most common cysts of the jaw, accounting for 54.6% of all odontogenic cysts. (3) After pulpal necrosis, apical inflammation can cause stimulation and proliferation of residual epithelial cells in the periodontal ligament. (4) The progression of this inflammatory stimulation leads to periapical cyst formation. Treatment consists of enucleation of the cyst lining coupled with root canal therapy and, in some instances, apicoectomy (surgical exposure of the root apex followed by its amputation and then obturation of the pulp canal opening). (4)
The aim of this case report is to demonstrate the success of concomitant cyst enucleation and bone grafting to correct a periodontal defect, along with SECT grafting to correct Miller Class III recession.
Case presentation and clinical examination
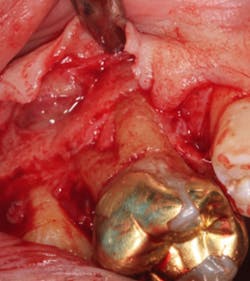
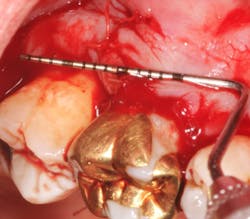
A 69-year-old male with a noncontributory medical history presented with 5 mm of recession, less than 1 mm of attached gingiva, and cervical notching on tooth No. 3. The tooth had an existing gold onlay and was caries-free (figures 1a and 1b). Radiographic analysis showed periodontal bone loss and a radiolucency at the apex of the tooth. The patient denied implant therapy and wanted to save the tooth.
Enucleation of cyst
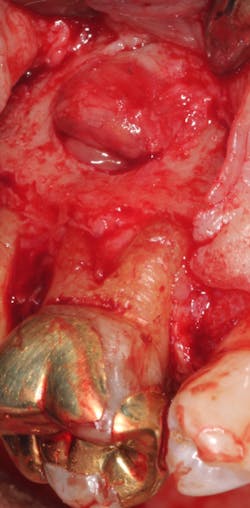
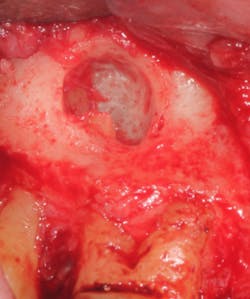
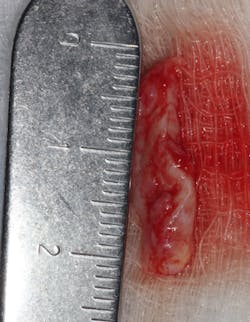
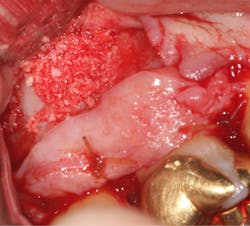
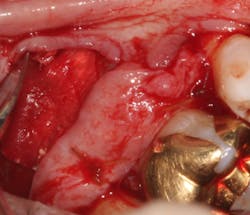
A split- to full-thickness intrasulcular incision was made on the facial of teeth Nos. 2 through 4. Upon completion of flap elevation, an intraosseous cyst associated with the distobuccal root of No. 3 was noted perforating the buccal plate and adherent to the overlying flap (figure 2). A sharp dissection separated the cyst from the flap (figure 3), and the cyst—measuring roughly 1.0 x 0.75 x 0.5 cm—was enucleated intact, leaving an intraosseous defect (figures 4a and 4b).
Grafting
A SECT graft was harvested from the palate (figure 5), and a periosteal-releasing incision was made to ensure flap advancement (figure 6). The SECT graft was secured on the facial of Nos. 2 and 3 with 4-0 chromic gut sutures (figure 7). The osseous defect was then grafted with mineralized cortico-cancellous particulate allograft (Puros, Zimmer Biomet Dental) and covered with a collagen membrane (Bio-Gide, Geistlich Biomaterials; figures 8a and 8b). The flap was coronally advanced to completely cover the hard- and soft-tissue graft and secured with 4-0 chromic gut sutures (figure 9). The palatal donor site was sutured with 4-0 chromic gut sutures as well (figure 10).
The patient received standard postoperative instructions: amoxicillin 500 mg bid for seven days, and ibuprofen 800 mg prn for pain.
Endodontic therapy
Nonsurgical endodontic therapy was completed within two weeks, and the patient ultimately received a full-coverage restoration (figure 11). The patient exhibited normal, uneventful postoperative healing.
Case assessment
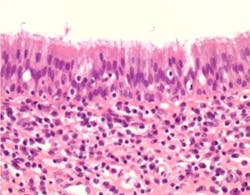
The pathology report identified the specimen as a 1.1 x 0.8 x 0.5 cm inflammatory cyst of the maxilla (figure 12). The patient now exhibits 10 mm of attached gingiva on the facial of tooth No. 3. The recession defect has been completely eliminated by a combination of the SECT graft and the full-coverage restoration (figure 13). The periapical radiograph shows no residual periapical pathology. After one year, the patient continues to be asymptomatic and is functioning well with the tooth.
This case demonstrates how proper periodontal-endodontic therapy is able to save teeth that have a guarded prognosis, thus eliminating the need for extraction. Tooth-replacement options involving implant therapy can often be more costly in the posterior maxilla, especially when sinus proximity is an issue and there is a need for sinus lifting.
Editor's note: Join us for the not-to-miss Perio-Implant Advisory Symposium on October 23, 2020. In this important virtual meeting, you’ll learn the newest skills it takes to save patients’ natural dentition. Bring your team and transform your practice. Conference schedule and special rates available at this link. Presented by Geistlich Biomaterials.
References
1. Informational Paper: Oral Reconstructive and Corrective Considerations in Periodontal Therapy. J Periodontol. 2005;76(9):1588-1600. doi: 10.1902/jop.2005.76.9.1588.
2. Tatakis DN, Chambrone L, Allen EP. Periodontal soft tissue root coverage procedures: a consensus report from the AAP regeneration workshop. J Periodontol. 2015;86(2S):S52-S55. doi: 10.1902/jop.2015.140376.
3. Johnson NR, Gannon OM, Savage NW, Batstone MD. Frequency of odontogenic cysts and tumors: a systematic review. J Investig Clin Dent. 2014;5(1):9-14. doi: 10.1111/jicd.12044.
4. Scholl RJ, Kellet HM, Neumann DP, Lurie AG. Cysts and cystic lesions of the mandible: clinical and radiologic‐histopathologic review. Radiographics. 1999;19(5):1107-1124. doi: 10.1148/radiographics.19.5.g99se021107.