Bone augmentation: Failures and complications
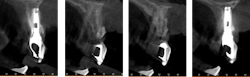
Failures and complications associated with bone augmentation can have a devastating effect on the outcome of dental implant treatment. These complications are classified as either early or late. Early complications include wound dehiscence, membrane and graft exposure, and infection, with the most common complication being wound dehiscence (figures 1a–1c). A strong correlation has been shown between flap tension and wound dehiscence, with wound breakdown occurring in 40% of cases where the flap tension reached 40.1 N as opposed to 10% for flap tensions < 0.1 N.1
Figures 1a–1c: Wound dehiscence occurring after bone augmentation procedures.
Other important etiologies for early soft-tissue breakdown include a lack of osteogenic potential of the recipient defect and soft-tissue reaction to the biomaterials used. While wound dehiscence and graft exposure result in an undesirable complication, their overall influence on the outcome of the augmentation procedure is controversial. Some studies have reported a significant increase in graft resorption with wound dehiscence compared to nondehisced sites; others have reported no effect on graft outcome.2 The overall effect of graft exposure will depend on several important variables: timing of exposure, soft-tissue biotype, technique employed, type of membrane or bone graft used, and type of recipient bone defect.
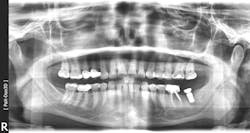
Late complications of bone augmentation are now recognized more frequently and include late resorption, foreign body reaction (figures 2a–2b), late breakdown of grafted sites (figures 3a–3e), lack of keratinized tissue and poor esthetics, as well as implant failure. While all bone augmentation procedures result in some degree of bone remodeling and resorption, significant late graft resorption can jeopardize the supporting bone around an already integrated implant, resulting in implant dehiscence, peri-implant disease, and late implant failure (figures 4a–4c). The degree of resorption depends on three important factors: alveolar defect configuration, patient factors, and the technique and grafting materials chosen.3
Figures 2a–2b: 12 years after ridge augmentation and implant placement. Breakdown of graft and biomaterial used resulted in a foreign body reaction and peri-implant infection.
Figures 3a–3e: Socket preservation was performed at the site of the left mandibular second molar after extraction, using a biomaterial two years prior to implant placement. Six years after implant placement, sequestration of the biomaterial is seen, resulting in peri-implant infection and failure of the implant.
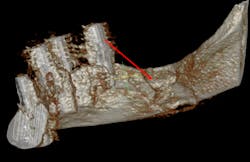
In addition to patient-related factors, a site-specific negative effect on bone healing has also been suggested. Sites of previous implant or graft failure will have compromised alveolar bone quality and quantity compared with unoperated sites. Thus, significantly lower survival rates of implants placed in sites of previous failure have been reported compared to initial implants, supporting evidence of site factors for failures.5 This site-specific theory is further supported by the finding that failed implants are often found in patients who have also had successful implants placed at other sites (figures 5a–5c).
Figures 5a–5c: Successive implant failures and bone augmentation in the right posterior mandible, resulting in compromised bone healing and subsequent chronic osteomyelitis.
Synopsis of Dr. Le’s presentation at the Academy of Osseointegration’s 2020 Annual Meeting
This clinical presentation will focus on how to identify and avoid potential complications before they arise, with emphasis given to risk assessment, classification of complications, and treatment of challenging failures. At the conclusion of this presentation, participants will be able to identify patient-related risk factors as well as site-related risk factors associated with bone augmentation procedures. The discussion will also include a strategic approach for the management of these challenging complications to minimize catastrophic failures.
For more information about the Academy of Osseointegration’s 35th Annual Meeting in Seattle, March 18–21, 2020, including speakers and activities, visit ao2020.osseo.org.
Author's note: Dental professionals can hear Dr. Le’s full presentation on this topic, “Bone Augmentation — Failures and Complications,” by attending the Academy of Osseointegration’s 2020 Annual Meeting. The meeting, “Evolving Technologies in Implant Dentistry,” will be held March 18–21, 2020, at the Washington State Convention Center in Seattle, Washington. Dr. Le will present his topic as part of the Academy’s Morning With the Masters series on Friday, March 20. Advance registration is available through February 24. For all meeting details, including online registration, please go to ao2020.osseo.org.
References
1. Burkhardt R, Lang NP. Role of flap tension in primary wound closure of mucoperiosteal flaps: a prospective cohort study. Clin Oral Implants Res. 2010;21(1):50-54. doi:10.1111/j.1600-0501.2009.01829.x.
2. Garcia J, Dodge A, Luepke P, Wang HL, Kapila Y, Lin GH. Effect of membrane exposure on guided bone regeneration: a systematic review and meta-analysis. Clin Oral Implants Res. 2018;29(3):328-338. doi:10.1111/clr.13121.
3. Elnayef B, Porta C, Suárez-López Del Amo F, Mordini L, Gargallo-Albiol J, Hernández-Alfaro F. The fate of lateral ridge augmentation: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 2018;33(3):622-635. doi:10.11607/jomi.6290.
4. Granate-Marques A, Polis-Yanes C, Seminario-Amez M, Jané-Salas E, López-López J. Medication-related osteonecrosis of the jaw associated with implant and regenerative treatments: systematic review. Med Oral Patol Oral Cir Bucal. 2019;24(2):e195-e203. doi:10.4317/medoral.22691.
5. Agari K, Le BT. Successive reimplantation of dental implants into sites of previous failure. J Oral Maxillofac Surg. 2019 Oct 13 [online ahead of print]. https://doi.org/10.1016/j.joms.2019.10.001. doi:10.1016/j.joms.2019.10.001.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a newsletter for dentists and hygienists that focuses on periodontal- and implant-related issues. Perio-Implant Advisory is part of the Dental Economics and DentistryIQ network. To read more articles, visit perioimplantadvisory.com, or to subscribe, visit dentistryiq.com/subscribe.
About the Author

Bach Le, DDS, MD, FACD, FICD
Bach Le, DDS, MD, FACD, FICD, completed his specialty training in oral and maxillofacial surgery at Oregon Health Sciences University and is currently clinical associate professor at the Herman Ostrow School of Dentistry at the University of Southern California. Dr. Le has authored more than 14 chapters in textbooks on bone regeneration and dental implants and has published extensively in peer-reviewed journals. He has been an invited speaker at numerous organizations, including the American Association of Oral and Maxillofacial Surgeons (AAOMS), Academy of Osseointegration, Academy of Prosthodontics, American Academy of Esthetic Dentistry, American Academy of Implant Dentistry, American College of Prosthodontists (ACP), Greater New York Academy of Prosthodontists, and the International Congress of Oral Implantologists. Dr. Le was inducted as an honorary member of the ACP and is a recipient of the Charles E. English Award in Clinical Science and Techniques. He is a diplomate of the AAOMS and holds a fellowship in the American College of Dentists, the International College of Dentists, and the International Association of Oral and Maxillofacial Surgeons.