Implant malposition: A simple clinical technique for prevention
Dental implants have proven to be very successful in the literature for the replacement of missing or hopeless teeth.1 Complications do occur, however, and dental implants can suffer from prosthetic or biologic problems over their years in service.2 In addition, as shown in the literature, the number of implants ailing or failing increases with the number of years postplacement.3
There are many reasons why dental implants ail or fail, with the most common complication arising from misplacement of the dental implant fixture at the time of placement.4 One study suggests that more than 40% of implants can be placed too far buccally and that the odds ratio of developing peri-implant disease from a misplaced implant is 48.2 (confidence interval of 11–204).5
Prosthetically driven implant therapy has been the goal of surgical dental implant therapy for well over two decades. There are many methods the restoring dentist can use to correct misplaced implants so as to achieve proper tooth anatomy and emergence profile.6
A good dental laboratory can also fabricate corrective abutments and frameworks that compensate for poor implant placement. Although restorative and laboratory correction are possible, the best method continues to be prevention by placing the dental implant in the proper position at the time of surgery. Surgical guides, computer-/satellite-aided software, and good treatment planning have all decreased the percentage of misplaced implants.7
. Furthermore, using a twist drill to correct position of the osteotomy might induce damaging thermal temperatures to the bone, especially in dense bone.8
Quick clinical technique to correct implant malposition
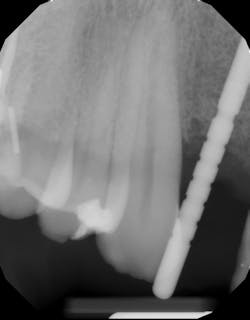
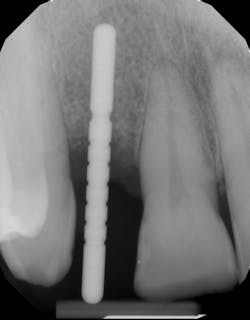
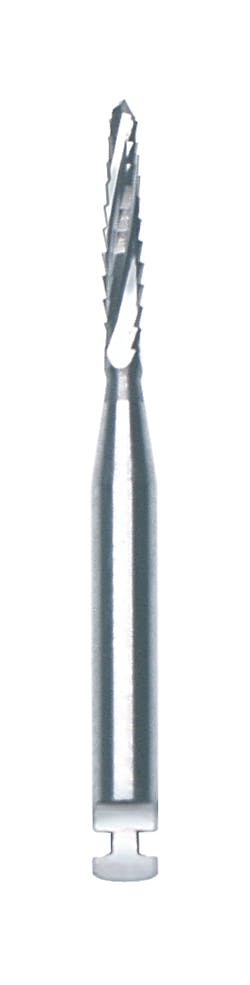
A quick clinical intervention to rectify incorrect initial osteotomy preparation can be accomplished with a Lindemann bur. A Lindemann bur is a side-cutting bur used to move pilot preparation in a bodily manner with ease and without the likelihood of further angulation issues (figure 4). After initial pilot drilling, a radiographic locator is placed to check position. If the radiographic index is shown to be incorrect, under copious irrigation, place a Lindemann bur in the osteotomy parallel to the intended location and move in a rigid upright fashion to the ideal location. Take a radiograph to verify correct position.
Lindemann burs offer an easy, inexpensive method to surgically correct a potentially large (and expensive) problem. They can be purchased from a variety of vendors, including Salvin Dental Specialties.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
References
- Moraschini V, da C Poubel LA, Ferreira VF, dos SP Barboza E. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. Int J Oral Maxillofac Surg. 2015;44(3):377-388. doi:10.1016/j.ijom.2014.10.023
- De Angelis F, Papi P, Mencio F, Rosella D, Di Carlo S, Pompa G. Implant survival and success rates in patients with risk factors: results from a long-term retrospective study with a 10 to 18 years follow-up. Eur Rev Med Pharmacol Sci. 2017;21(3):433-437.
- Simonis P, Dufour T, Tenenbaum H. Long‐term implant survival and success: a 10–16‐year follow‐up of non‐submerged dental implants. Clin Oral Implants Res. 2010;21(7):772-777. doi:10.1111/j.1600-0501.2010.01912.x
- Monje A, Galindo-Moreno P, Tözüm TF, Suárez-López del Amo F, Wang HL. Into the paradigm of local factors as contributors for peri-implant disease: short communication. Int J Oral Maxillofac Implants. 2016;31(2):288-292. doi:10.11607/jomi.4265
- Canullo L, Tallarico M, Radovanovic S, Delibasic B, Covani U, Rakic M. Distinguishing predictive profiles for patient-based risk assessment and diagnostics of plaque induced, surgically and prosthetically triggered peri-implantitis. Clin Oral Implants Res. 2016;27(10):1243-1250. doi:10.1111/clr.12738
- Chatterjee A, Ragher M, Patil S, Chatterjee D, Dandekeri S, Prabhu V. Prosthetic management of malpositioned implant using custom cast abutment. J Pharm Bioallied Sci. 2015;7(Suppl 2):S740-S745. doi:10.4103/0975-7406.163528
- Arisan V, Karabuda ZC, Ozdemir T. Accuracy of two stereolithographic guide systems for computer-aided implant placement: a computed tomography-based clinical comparative study. J Periodontol. 2010;81(1):43-51. doi:10.1902/jop.2009.090348
- Bernabeu-Mira JC, Pellicer-Chover H, Peñarrocha-Diago M, Peñarrocha-Oltra D. In vitro study on bone heating during drilling of the implant site: material, design and wear of the surgical drill. Materials (Basel). 2020;13(8):1921. doi:10.3390/ma13081921
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.