5 questions to ask when determining if teeth with perio-endo infections can be saved
Editor's note: Originally published May 8, 2017. Updated for clinical accuracy February 15, 2022.
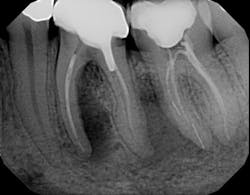
Many clinicians struggle with the question of whether a tooth experiencing an infection from an endodontic, periodontic, or combination lesion is worth trying to save. These teeth may require root canal, periodontal, and restorative therapy. Is it worth it to try to treat and save the tooth versus taking it out and placing a dental implant or bridge? This article will guide you through this decision by explaining how to diagnose the infection and suggest questions you should ask when deciding upon the method of treatment.1. What is the etiology of the infection?
a. Treatment is dictated by etiology; furthermore, so is prognosis
2. What is the clinical/radiographic presentation?
a. How mobile are the teeth: Class I, II, or III?
b. How severe is the probing: less than 5 mm, 5–8 mm, or greater than 8 mm
c. Is the furcation involved if multirooted teeth? If so, is it Class I, Class II, or Class III?
d. Is the bone loss vertical or horizontal, and what is the severity?
e. Is there a sinus tract and/or edema present?
3. Restorability: Can the tooth be restored with a restoration that will last?
a. Can coronal and radicular dentin be preserved after caries removal?
b. Can contamination of the root canal system be avoided?
c. Can a proper post and core be placed without causing root fracture?
d. Is adequate ferrule present?
e. Is adequate interocclusal space present to allow for crown placement?
f. Is crown lengthening needed, and if so, how much reduction is necessary?
4. What are the costs and compliance involved?
a. Can the patient afford treatment by multiple specialists?
b. What are the anticipated maintenance fees?
c. Is the patient motivated, and will the patient comply with long-term follow-up?
5. What are the alternative treatment options to present to the patient?
a. Hemisection/bicuspidization of multirooted teeth
c. Guided tissue regeneration
d. Extraction and subsequent implant therapy
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.
Marcus Johnson, DDS, MSD
Marcus Johnson, DDS, MSD, is a graduate of Rutgers University and New York University Dental School. He received his Certificate of Endodontics from Case Western Reserve University, while concurrently earning his master’s degree in dentistry. Dr. Johnson, an astute evidence-based clinician and an active member of numerous dental organizations, won an award for his research on new treatment techniques. He is the lead attending endodontist for the general practice residency at Interfaith Medical Center in Brooklyn, New York, where he also teaches the pediatric residents. He is a member of the American Association of Endodontists’ board of directors, a diplomate of the American Board of Endodontics, and president of the New York State Association of Endodontists. As a board-certified endodontist, Dr. Johnson owns and operates City Endodontics, a private practice specializing in endodontics in Manhattan.