Saving teeth: Revisiting molar furcation treatment with advanced technology
Although dental implants have been shown to be a reliable tooth-replacement option in the literature, a priority should be directed at saving and restoring the natural dentition, if possible. There are many considerations that determine the prognosis of a tooth, such as caries involvement, endodontic involvement, restorability, strategic position of the tooth in the arch, patient history, occlusion, and periodontal support. Periodontal support is a major determinant in whether a tooth is saved or extracted.
Recent studies suggest that the threshold for tooth extraction in favor of dental implant therapy is too low. One study suggests that anterior incisors with 50% bone loss, premolars with 48% bone loss, and molars with 42% bone loss are likely to be extracted instead of saved with periodontal therapy.1 Other studies suggest that this threshold of tooth extraction is lowered further once a molar furcation is exposed, even though furcation treatment modalities have become more predictable with advanced technology. In addition, some studies suggest the cost of regenerating and maintaining natural teeth with furcations is lower than the placement and maintenance of dental implants over a long period of time.2 This article will briefly review the classification of molar furcation, prognosis, and highlight new technology that can change the extract versus save decision matrix.
Classification of molar furcation
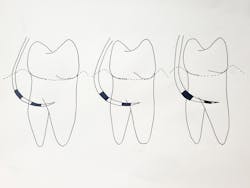
There are numerous classification systems that categorize molar furcations based on the degree of involvement. The Modified Hamp Classification System is one that is quite easy to use. It requires the clinician to use a periodontal probe and place it into the furcation to measure the horizontal depth of insertion3 (figure 1).
Class I furcations are classified by horizontal bone loss that is less than 3 mm as measured by a periodontal probe. These types of furcations are usually treated by debridement and/or bur odontoplasty to make them more cleansable for the patient.4
Class II furcations are classified by horizontal bone loss that is greater than 3 mm as measured by a periodontal probe. Recent literature suggests that most maxillary and mandibular grade II furcations can be regenerated predictably with good surgical technique and have a good prognosis.5 Unfortunately, according to a recent review by Pjetursson et al., common sentiment among many clinicians on lecture circuits and social media is that implants have a better outcome in these situations, and extraction therapy has a better long-term prognosis.6
Class III furcations are classified by horizontal bone loss that allows the periodontal probe to go through the furcation to the other side of the tooth, demonstrating no bone in the furcation, or what is known as a “through-and-through defect.” Class III furcations are especially difficult to treat, and most prognosis systems label these teeth as hopeless and recommend extraction.7
Because tooth prognosis is usually determined by response of the teeth in question to treatment protocols and the projected long-term survival rate, if advances in technology could address limitations of furcation treatment, it may be possible to change the prognosis.
3 technology solutions to change the extract versus save decision matrix
There are three main limitations during the treatment of furcations that can affect prognosis and influence a clinician in the save-extract decision matrix.
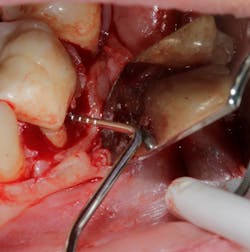
No. 1—Instrument access into the entrance of the furcation is limited. Anatomical evaluation suggests that most furcation entrances are less than 1 mm in width and most hand scalers are greater than 1 mm in width, preventing instrument access (figure 2).
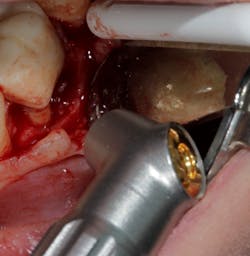
Technology solution: Many dental lasers can focus their beam smaller than 1 mm to enter the furcation for detoxification.8 For example, a 9.3-micron CO2 laser has a spot size of the focal laser beam in the control range of .25 mm–1.25 mm so the beam can be directed into the furcation entrance, which allows previously difficult furcal defects to be detoxified prior to regenerative therapy. Because of this enhanced ability to detoxify, this laser has been able to change the prognosis of once hopeless teeth (figure 3) and allow for tissue regeneration instead of extraction.
No. 2—The anatomy of the roots in the furcation are often concave and very hard to instrument, even if access to the furcation is possible (figure 4).
Technology solution: Many commercially available lasers have handpieces with tips capable of side firing and/or radial firing. This would be similar to an umbrella opening up or being in a cave and having the ability of a flashlight to completely illuminate in a 360-degree direction. In other words, the laser has the capability to penetrate all areas and convexities harboring the bacteria that is preventing proper detoxification/tissue regeneration.
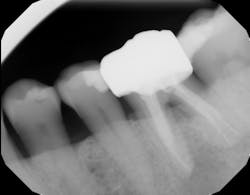
No. 3—The furcal area has a poor blood supply and space-maintaining ability, so conventional grafts are unlikely to be successful in this area.
Technology solution: Commercially available bone grafts, such as Geistlich Bio-Oss Collagen, can have components that make them space maintaining as well as act as polymers to absorb and release growth factors and proteins (figure 5). By adding growth-stimulating factors/proteins to your regular bone grafts (figure 6), an increase in osteopromotive potential occurs that can have the ability to overcome a deficiency of bone walls.9 In other words, your bone graft can become alive, and furcations that once were unable to be repaired (figure 7) now have a more predictable success rate10 (figure 8).
In summary, advancements in technology have given clinicians the ability to access difficult furcal defects and allow for detoxification of bacteria. In addition, challenging Class II–III furcal defects that have few remaining bony walls can now be overcome with increased osteoblastic activity of bone grafts containing added growth-stimulating factors. The combination of these two advancements have allowed clinicians to save molar teeth that were once planned for extraction.
Editor's note: Join us for the not-to-miss Perio-Implant Advisory Symposium on October 23, 2020. In this important virtual meeting, you’ll learn the newest skills it takes to save patients’ natural dentition. Bring your team and transform your practice. Conference schedule and special rates available at this link. Presented by Geistlich Biomaterials.
References
1. Splieth C, Giesenberg J, Fanghanel J, Bernhardt O, Kocher T. Periodontal attachment level of extractions presumably performed for periodontal reasons. J Clin Periodontol. 2002;29(6):514-518. doi:10.1034/j.1600-051x.2002.290607.x.
2. Ntolou P, Prevezanos I, Karoussis IK. Prognosis of furcation involved teeth: Cost-effectiveness over implant placement. Dent Health Curr Res. 2016;2:3. doi:10.4172/2470-0886.1000121.
3. Hamp SE, Nyman S, Lindhe J. Periodontal treatment of multi rooted teeth. Results after 5 years. J Clin Periodontol. 1975;2(3):126-135. doi:10.1111/j.1600-051x.1975.tb01734.x.
4. Reddy MS, Aichelmann-Reidy ME, Avila-Ortiz G, et al. Periodontal regeneration – furcation defects: a consensus report from the AAP Regeneration Workshop. J Periodontol. 2015;86(suppl 2):S131-S133. doi:10.1902/jop.2015.140379.
5. Avila-Ortiz G, De Buitrago JG, Reddy MS. Periodontal regeneration – furcation defects: a systematic review from the AAP Regeneration Workshop. J Periodontol. 2015;86(suppl 2):S108-S130. doi:10.1902/jop.2015.130677.
6. Pjetursson BE, Heimisdottir K. Dental implants – are they better than natural teeth? Eur J Oral Sci. 2018;126(suppl 1):81- 87. doi:10.1111/eos.12543.
7. Nunn ME, Fan J, Su X, Levine RA, Lee HJ, McGuire MK. Development of prognostic indicators using classification and regression trees for survival. Periodontol 2000. 2012;58(1):134-142. doi:10.1111/j.1600-0757.2011.00421.x.
8. de Andrade AK, Feist IS, Pannuti CM, Cai S, Zezell DM, De Micheli G. Nd:YAG laser clinical assisted in class II furcation treatment. Lasers Med Sci. 2008;23(4):341-347. doi:10.1007/s10103-007-0482-6.
9. Sharma A, Pradeep AR. Autologous platelet-rich fibrin in the treatment of mandibular degree II furcation defects: a randomized clinical trial. J Periodontol. 2011;82(10):1396-1403. doi:10.1902/jop.2011.100731.
10. Casarin RC, Ribeiro Edel P, Nociti FH Jr, et al. Enamel matrix derivative proteins for the treatment of proximal class II furcation involvements: a prospective 24-month randomized clinical trial. J Clin Periodontol. 2010;37(12):1100-1109. doi:10.1111/j.1600-051X.2010.01614.x.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and dental hygienists for issues relating to periodontal and implant medicine. Exclusive content from an academic perspective centers on complex care, solving clinical complications from a team-based approach through interdisciplinary management.
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.