Quest for the best dental bonding agent
Based on the presentation at the McLean Memorial Lecture, London, 2010
In the Buonocore Memorial lecture in 2003, Van Meerbeck and colleagues stated “... the data presented confirm that conventional three-step etch-and-rinse adhesives still perform most favorably and are most reliable in the long term. Nevertheless, a self-etch approach may have the best future perspective.” (1) Now, considering the rapid progress of self-etching bonding agents, we might wonder if these statements are still true about seven years later.
Indeed, in a very recent paper, (2) Van Meerbeek states, “When bonding to enamel, an etch-and-rinse approach is definitely preferred, indicating that simple micro-mechanical interaction appears sufficient to achieve a durable bond to enamel. When bonding to dentin, a mild self-etch approach is superior, as it involves (like with glass-ionomers) additional ionic bonding with residual HAp. This additional primary chemical bonding definitely contributes to bond durability. Altogether, when bonding to both enamel and dentin, selective etching of enamel followed by the application of the two-step self-etch adhesive to both enamel and dentin currently appears the best choice to effectively and durably bond to tooth tissue.”
Self-etching primers have displaced etch-and-rinse systems in the dental market in many regions of the world, now more than 85% of the market share in Japan. In addition to the obvious simplification in clinical procedures, it appears that a major part of this trend toward self-etching primers is attributable to the well-known fact that self-etching primers are far less prone to result in postoperative sensitivity than are etch-and-rinse systems. The probable reason for lack of sensitivity is that the smear plugs in the tubules are not removed by the self-etching primer, contrary to their removal by etch-and-rinse. Another compelling reason to use self-etching systems is better dentin bond stability. (3)
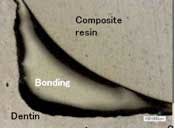
Current thinking is that the self-etching primers, unlike typical etch-and-rinse systems, do not demineralize dentin deeper than can be completely hybridized with infused primer and bonding agent. Overetched and unhybridized dentin is a source of nanoleakage, with ingress of water that is thought to cause hydrolytic breakdown of the demineralized layer, resulting in bond instability typically observed with etch-and-rinse systems.
One concern is for the ability of self-etching systems to produce a strong and durable enamel bond. Due to major differences in acidity of the primers, the enamel bonding ability varies greatly among products. Clinical reports in the literature are sometimes contradictory for a particular product. However, it is generally agreed that separate phosphoric acid etch and rinse of the enamel will improve the bond of most, if not all, self-etching primers. An analogous improvement in dentin bond is not expected since the separate etching will tend to over-etch, creating an etched and nonhybridized layer of dentin beneath the hybridized layer. (4)
“Immediate dentin sealing” (5,6)for indirect restorations is now being utilized at an increasing rate. As CAD/CAM restorations become more commonly used, another major consideration is the thickness of the bonding layer. For clinical efficiency, it is highly desirable to make the “optical impression” immediately after preparation and then apply the dentin bond clean dentin in a sufficiently thin layer so as to preclude blocking the fit of the milled restoration. Applying the dentin seal even 30 minutes before final bonding of the restoration will reduce stresses on the dentin bond significantly.
With the above factors in mind, here is a list of the properties that a “dream bond” would have:
- Work in self-etch or etch-and-rinse modes
- High SE early enamel bond strength
- High SE early dentin bond strength
- SE ability on uncut enamel
- Bond to enamel/dentin/metal/ceramic for repairs
- No bond to metal matrix
- Bond stability on dentin and enamel
- No “transudation”
- Form an acid-base resistant zone ahead of the hybrid layer
- LC, SC, DC compatible
- Minimal technique sensitivity
- Not visible on X-ray as radiolucency (very thin or radiopaque)
- Solvents easily evaporated
- Shelf-life stable
- Both direct composite and CAD/CAM friendly (very thin, dual-cure)
The last requirement for dream bond — that it be very thin and dual cure — eliminates the majority of self-etching systems. Only two self-etching systems have been observed by the author to be very thin ... sufficiently thin as to not interfere with the fit of CAD/CAM restorations (e.g., CEREC), assuming a fit tolerance of 100 microns. These are Bond Force (Tokuyama) and Prelude SE (Danville). All other bonds observed are too thick to meet this requirement (e.g., Clearfil SE Bond). Radiolucency of thick bonds is another consideration. Evaluation of bond thickness in the corners of preparations, rather than on a flat surface (as manufacturers usually do), is thought to be more clinically relevant to actual tooth preparations.
Prelude SE is a dual-cure bonding agent, whereas Bond Force is a light-cure-only bonding agent. Use of one-bottle Bond Force is easier than Prelude SE, but the light-cure-only capability may complicate its use for indirect restorations. The following specimens were made using the manufacturer's instructions for use of the bonding agents.
Clearfil SE Bond (Kuraray)
The SE Bond appears to make an excellent adaptation to the tooth preparation. However, its high thickness, especially in the pooled corners, makes it too thick for typical CAD/CAM restorations where immediate dentin sealing is done after the optical impression.
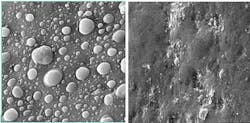
Some other bonds observed suffer from a variety of problems. For example, Xeno IV and AdheseOne show poor adhesion and incomplete sealing in the corners of a tooth preparation. Solvent removal appears to be a problem with Clearfil S. (3) Phase separation appears to be a problem with G Bond. Also, the acetone solvent in G Bond evaporates very fast and the bonding resin becomes very sticky, preventing application of a thin layer.
Acknowledgement: The author thanks Dr. S. Inokoshi for specimen preparation and Mr. Matsushige at Tokuyama for the images.
Transudation (7) — that is, permeation of pulpal fluids through the hybrid layer — is a problem common to all of the one-bottle self-etching systems. In contrast, the two-layer systems do not exhibit transudation due to the sealing ability of the water-free, hydrophobic second layer. While transudation can be sufficiently managed, it appears that two-layer systems would be less technique sensitive.
Acknowledgement: The author thanks Dr. F. Tay for these images.
Recent research by Tagami (8)and colleagues has shown that self-etching primers can produce a protective acid-base resistant zone in dentin, below the hybrid layer. This is yet another good reason to use self-etching primers.
Considering lack of transudation, a remarkably thin bond layer, no transudation, and universal compatibility (LC, SC, DC), a good case can be made for selecting Prelude SE. With the exception of metal and ceramic bonding for repairs, Prelude SE satisfies all of the requirements for a “dream bond” as outlined above. (Metal bonding would be to a metal matrix too.) It may be used as a self-etching system or as an etch-and-rinse system, omitting use of the self-etching primer and instead using phosphoric acid etchant. The clinical results are about the same for most cavity preparations. When visible margins are involved, the phosphoric etch is expected to enhance the durability of the bond.
In summary, current thinking is that the technique simplification, improved dentin bond durability, lack of postoperative sensitivity, and excellent clinical results make a good case for using the best self-etching primer systems rather than etch-and-rinse systems. Prelude SE appears to be an optimal choice when used in the self-etching technique for posterior restorations and with etch-and-rinse (omitting use of the self-etching primer) in visible margin anterior restorations.
Author bio
Raymond L. Bertolotti, DDS, PhD, received his DDS degree from the University of California, San Francisco, after working as a PhD metallurgical and ceramic engineer at Sandia National Laboratories. He is currently visiting honorary professor at Warwick University in the U.K. and is a guest lecturer at Loma Linda University. He maintains a private practice in California, largely involved with ozone, tooth-conservative esthetics, and adhesion dentistry. Dr. Bertolotti is perhaps best known for introducing “total etch” to North America in 1984. He also introduced Caries Detector in 1984, Panavia in 1985, tin-plating in 1989, self-etching primers in 1992, and ozone dentistry in 2004. The sectional Contact Matrix system, "Microprime", "Microetcher” sandblasting, Accolade PV, and intraoral tin-plating are among his innovations. He has published extensively in various dental journals, as well as authored four dental textbook chapters. He is a fellow of the American Academy of Dental Materials, the American College of Dentists, the Pierre Fauchard Academy, and an accredited member of the Academy of Cosmetic Dentistry. Dr. Bertolotti has spoken at most of the major dental meetings. As a well-known international lecturer, he has given invited presentations in more than 30 countries. Visit his website at www.adhesion.com.
References
1. Van Meerbeek B et al. Buonocore Memorial Lecture. Adhesion to enamel and dentin: Current status and future challenges. Oper Dent 2003; 28:215-235.
2. Van Meerbeek B et al. Relationship between bond-strength tests and clinical outcomes. Dent Mater 2010; 26:100-121.
3. Burrow MF et al. Seven-year dentin bond strengths of a total- and self-etch system. Eur J of Oral Sci 2005; 113:265-270.
4. Walker et al. Influence of additional acid-etch treatment on resin cement dentin infiltration. J Prosth 2000; 9:77-81.
5. Jayasooriya PR et al. The effect of a “resin coating” on the interfacial adaptation of composite inlays. Oper Dent 2003; 28-35.
6. Magne P et al. Immediate dentin sealing supports delayed restoration placement. J Prost Dent 2007; 98:166-174.
7. King NM et al. Conversion of one-step to two-step self-etch adhesives for improved efficacy and extended application. Am Journal Dent 2005; 18:126-134.
8. Nikaido T et al. Assessment of the nanostructure of acid-base resistant zone by the application of all-in-one adhesive systems: Super dentin formation. Bio-Medical Materials and Engineering 2009; 19(2-3):163-171.