Prosthetic management of surgical complications using e.max
By Amanda Seay, DDS Esthetic challenges ... There are many situations when a patient presents with bone and tissue defects that are very difficult to correct. A young male patient, 36 years old, presents with injuries from a traumatic car accident several years ago. He fractured teeth Nos. 7 through 10. No. 10 was extracted and an implant placed; root canals were done on Nos. 7, 8, and 9. Unfortunately, there was a lack of planning and the implant failed due to poor position. The patient was also unhappy with the esthetics of his crowns — the color was flat, opaque, and unnatural — and he also disliked the diastema he had between his teeth.
This young man came to me with the desire to restore his teeth to function since the implant was failing. While he knew something had to be done functionally, he also desired a different esthetic outcome if possible. When I saw his case, I was struck by the size of the bone and tissue defect that was already present with a failing implant in place. The first step was to do a smile analysis. It may seem contrary to look at esthetics before function, but we always need to know what our esthetic goal is, so we can try to engineer everything to make it happen. From there, the esthetic goal is communicated to the surgeon to try to achieve correct implant placement to make the esthetics of that implant possible. In this patient’s case, a bone and tissue graft were done after the implant was removed. After several months, the new implant was placed. Again, we had to wait a few more months to allow osseous integration to see how much bone and tissue graft would resorb or be lost. Although the grafting helped make a new implant possible, the tissue was still severely deficient, and we were faced with managing difficult tissue esthetics. The patient's gingival architecture was completely flat with no hope of establishing a nice scallop at the same tissue height of adjacent teeth. This patient also had a very high lip dynamic — an all-around high-risk esthetic case!
Where do we go from here? We still wanted to achieve the same esthetic goal we had planned in our smile analysis, but since we could not get the tissue graft to work for us, we had to look at other options. This is when communication between the dentist and lab technician is crucial. You need to have excellent photography to communicate the details to the lab technician, as well as a clear understanding of restorative materials and their capabilities. Upon several conversations with my lab technician, it was decided to use IPS e.max, a lithium disilicate glass ceramic that has optimized translucency, durability, and strength. Its opalescence, translucency, and light diffusion properties truly replicate natural tooth structure for beauty and undetectable restorations. We also decided to splint the two implant crowns instead of making single crowns. Why? Simple, because the two connected crowns could house the pink porcelain that is made to look like natural tissue and recreate the papilla the patient was lacking, especially in the area between teeth Nos. 9 and 10.
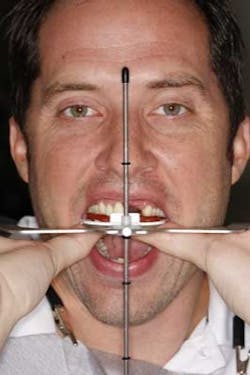
At the records appointment, I used a Kois facebow and photographs to record the position of the maxillary incisal edge, based on dentofacial esthetics.
Information was sent to the lab and the lab technician did a diagnostic wax-up. Siltech putty matrix was used to fabricate chairside provisionals.
I did careful shade mapping of the patient's gingival tissue and photographed several “pink” composite shades to let the lab technician know exactly what shade of pink to use to make it blend. Once the pink shade was selected, I made some pink composite disks in varying thicknesses and sent those directly to the lab. I also did an intraoral mockup with the pink composite.
The lab technician and I discussed the benefits of using pink composite bonded to the e.max restorations as a final restorative choice. This would give me more control over blending the composite and create a truly invisible margin. Drawbacks were that the pink composite could discolor over time and need repair (though it could be repaired easily at chairside). We decided on the pink porcelain since the patient had full display of his tissue and did not want to deal with the composite becoming discolored periodically. The result? A beautiful smile restored to full function and health. Notice how the pink porcelain blends into the patient's own tissue. The contour, color, and shape of the four crowns blend seamlessly into the rest of the smile. It has been a long, hard road for this young man, but he finally has the beaming smile he has always carried in his heart.
Author bio Dr. Amanda Seay is the owner and solo practitioner of Park West Dentistry, a private practice in Mount Pleasant, SC. A graduate of New York University College of Dentistry and both the Kois Center and The Pankey Institute, Dr. Seay commits herself to hundreds of hours of continuing education each year. In addition to operating a thriving full-time dental practice, she is the CEO of a family of six, including four children under the age of 7.