Fractured calculus and dental implant failure
Abstract
The reported incidence of abutment screw fracture is slightly less than 1%.1 Incomplete scaling and root planing, with fractured subgingival calculus, is responsible for much recurrent periodontal disease, and this impacts dental implant success rates. A recent study reported that dental implant failures are five times more likely in patients with recurrent periodontal disease than in those who are stable after treatment.2 In fact, when evaluating tooth loss due solely to periodontal disease, patients with chronic periodontal disease were 10 times more likely to keep their natural teeth versus teeth that were replaced with dental implants.
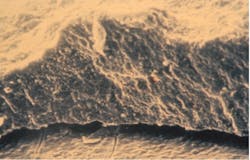
Scaling and root planing is very effective in reducing clinical inflammation and probing depths when the subgingival calculus is removed. Calculus will often remain depending on the pocket depth, root anatomy, furcation involvement, mode of attachment, the time spent in removal, and the operator’s skill and experience (figure 1).3
For decades, the beneficial effect of calculus removal on the resolution of inflammation has been well-known. Nevertheless, over the past several years, for a variety of reasons, clinicians, educators, and state board examiners have diminished the significance of complete calculus removal in favor of establishing a “biocompatible root surface” to achieve periodontal health. This, for some, is the removal of loosely attached biofilm and endotoxins, and some calculus. The critical question is: can a root surface with retained calculus be compatible with health?
High-powered transmission electron microscopic assay has revealed calculus to be a porous mineralized structure—like a dry sponge—allowing viableMultiple studies in the literature show a relationship between subgingival calculus, inflammation, and microulcerations in the adjacent soft-tissue wall of the periodontal pocket. The bacteria within the calculus have the potential to release potent toxins into the tissues, inciting inflammation and causing the disease to progress. Periodontal pathogens, such as Porphyromonas gingivalis, are capable of reaching the bloodstream through the ulcerated pocket wall and have been found in the brains of patients with Alzheimer’s and in coronary atheromatous plaques.
In addition to pathogenic bacteria living within and on the surface of retained calculus, other places where they can reside are the lamina propria of the pocket wall, the epithelium of the buccal mucosa, the dorsum of the tongue, tonsillar crypts, and saliva.6 All these sites may contribute to the pathogenic microbial flora associated with peri-implantitis in patients with poorly controlled periodontal disease.
Partially edentulous patients with a history of moderate-to-severe periodontitis have more peri-implant bone loss than those with a history of periodontal health. This contradicts the belief of many clinicians that simply extracting teeth with periodontitis involvement and placing implants can substitute for the establishment of prolonged periodontal health of the entire dentition.7
Subgingival calculus removal: A challenging situation
- Cemental mounds. These sessile elevations on the surface of cementum are the former insertion sites of the collagen fibrils of the periodontal ligament. The underside of calculus has depressions that fit over the mounds, providing minimal retention (figure 3). Light root planing with a curette or ultrasonic scaler is sufficient for removal.
- Resorption lacunae. These defects may be pervasive and may be formed by persistent occlusal trauma or orthodontic treatment.8 Rapidly advancing periodontitis allows pathogenic microbiota to invade, colonize, and harden. The resultant calculus can be attached into the lacunae, making removal without surgery very difficult.
- Fractured calculus. Calculus can chemically bond to the hydroxyapatite crystalline structure of cementum, and that union can be stronger than the cohesive strength within calculus itself.9 When attempting to remove, the calculus can fracture and a basal layer remains firmly attached to the root. Repeated strokes with a scaling instrument result in a “burnished,” or smooth, surface that is often undetectable by a periodontal probe.
Residual calculus and peri-implantitis
For a variety of reasons, dentists and hygienists may not be able to remove all the subgingival calculus and biofilm during scaling and root planing. This pathogenic ecosystem may not only be harmful to the individual tooth, but it can also be a source of the bacterial infiltrate found in the peri-implant environment.
A thorough reevaluation should be performed four to six weeks after scaling and root planing and prior to implant placement. This time frame is optimal because the trauma caused by the instrumentation will have resolved and any repopulation of residual bacteria will have reached sufficient numbers so that inflammation from microbial sources, if present, will be evident. This appointment should be separate from a periodontal maintenance visit and be of sufficient length to carefully measure all pocket depths and assess the level of inflammation. If pockets are still deep (5 mm and over) and bleed upon probing, further therapy is indicated. Since the clinician cannot see the root surface, gingival tissue health must be evaluated by vision and tactile means.
Clinical case report
A patient had four quadrants of scaling and root planing in the office of her general dentist. Subsequently, three maxillary anterior implants were placed. The patient was scheduled every six months for periodontal maintenance visits. Radiographs taken prior to the scaling and root planing (figure 4) revealed moderate periodontitis with slight vertical bone loss involving the mandibular left first molar. A deep vertical osseous defect on the distal of the second molar was present.
Conclusion
A preexisting periodontal condition should be controlled prior to the placement of dental implants. Fractured calculus may remain after scaling and root planing, and its removal may require surgery. Attaining periodontal health first may prevent a comorbidity and the potential loss of both teeth and implants. Placing implants into an oral cavity with unresolved periodontitis can result in a serious problem, while a fractured implant abutment screw is a minor one.Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
References
- Katsavochristou A, Koumoulis D. Incidence of abutment screw failure of single or splinted implant prostheses: a review and update on current clinical status. J Oral Rehabil. 2019;46(8):776-786. doi:10.1111/joor.12817
- Guarnieri R, Di Nardo D, Di Giorgio G, Miccoli G, Testarelli L. Longevity of teeth and dental implants in patients treated for chronic periodontitis following periodontal maintenance therapy in a private specialist practice: a retrospective study with a 10-year follow-up. Int J Periodontics Restorative Dent. 2021;41(1):89-98. doi:10.11607/prd.4674
- Heitz-Mayfield LJA, Trombelli L, Heitz F, Needleman I, Moles D. A systematic review of the effect of surgical debridement vs. non-surgical debridement for the treatment of chronic periodontitis. J Clin Periodontol. 2002;29(Suppl 3):92-102. doi:10.1034/j.1600-051x.29.s3.5.x
- Calabrese N, Galgut P, Mordan N. Identification of Actinobacillus actinomycetemcomitans, Treponema denticola and Porphyromonas gingivalis within human dental calculus: a pilot investigation. J Int Acad Periodontol. 2007;9(4):118-128.
- Cobb CM, Sottosanti JS. A re-evaluation of scaling and root planing. J Periodontol. 2021;1-9. Published online: March 4, 2021. doi:10.1002/JPER.20-0839
- Greenstein G, Lamster I. Bacterial transmission in periodontal diseases: a critical review. J Periodontol. 1997;68(5):421-431. doi:10.1902/jop.1997.68.5.421
- Gatti C, Gatti F, Chiapasco M, Esposito M. Outcome of dental implants in partially edentulous patients with and without a history of periodontitis: a 5-year interim analysis of a cohort study. Eur J Oral Implantol. 2008;1(1):45-51.
- Sottosanti JS. A possible relationship between occlusion, root resorption, and the progression of periodontal disease. J West Soc Periodontol Periodontal Abstr. 1977;25(2):69-74.
- Rohanizadeh R, Legeros RZ. Ultrastructural study of calculus-enamel and calculus-root interfaces. Arch Oral Biol. 2005;50(1):89-96. doi:10.1016/j.archoralbio.2004.07.001
About the Author

John Sottosanti, DDS
John Sottosanti, DDS, received his undergraduate education at the University of Pennsylvania and his DDS degree from Georgetown University. His postdoctoral education in periodontics was at the University of Southern California (USC) School of Dentistry and the West Los Angeles VA Medical Center. For 27 years, he chaired and moderated the Annual USC Periodontal Symposium. Dr. Sottosanti has done original research on biofilm, calculus, and bone regeneration and has been a speaker at many regional, national, and international dental meetings. He is a past-president of the California Society of Periodontists and was elected to the American College of Dentists and the Pierre Fauchard honor dental society. Dr. Sottosanti has had a private practice in periodontics and implantology in San Diego, California, for many years.